Introduction
Sciatic hyperalgesia (SH) is a type of chronic pain in the sciatic nerve distribution caused by constriction of the sciatic nerve at focal areas extending from the lower back to the foot . Chronic constriction of peripheral nerves by adjacent musculoskeletal structures leads to mechanical irritation and nerve ischaemia, which may increase abnormal neural sensitivity and lead to sensory motor dysfunction [2].
The factors influencing chronic sciatic nerve constriction are intervertebral disc bulge, tightness of the piriformis, hamstring, and deep calf muscles, and tarsal tunnel syndrome [3]. in individuals with hyperalgesia, even non-painful low-threshold touch, pressure, cold, and temperature can aggravate pain perception [4]. Pathophysiologically, mechanical pressure and inflammatory processes in the peripheral nerves are considered the primary causes of mechanical hyperalgesia [5].
Sciatica is common in adults, though hyperalgesic symptoms are rarely reported in regular clinical practice. The uniqueness of SH is that the sciatic nerve undergoes chronic constriction at multiple points from the lower back to the tarsal tunnel [6]. Therefore, it is difficult for clinicians to determine its exact cause and whether the compression is from a single point or multiple areas. Nerve root compression at the lower back, nerve trunk under/within the piriformis muscle, entrapment between the two heads of the biceps femoris, and tarsal tunnel are a few examples of multiple compressions of the sciatic nerve [7].
Studies have reported that sustained mechanical pressure from the adjacent musculoskeletal structures over the sciatic nerve produces an ischaemic crisis, which induces the release of neuroinflammatory sensitising substances, especially calcitonin gene-related peptides (CGRP), tumour necro- tising factors (TNFs), nor-epinephrine (NE), and Substance P.
These factors may be responsible for the development of local or widespread pain, hyperalgesia, allodynia, and a reduced pain threshold [5, 7]. in addition, increased abnormal neural sensitivity could lead to the shortening of muscle fibres and constriction of capillaries to form myofascial trigger points (MTrPs) that further lead to SH [8]. Similarly, Gunn’s radiculo- pathic model of trigger point formation suggests that sustained neural irritation plays a major role in the development of MTrPs in spinal and peripheral muscles [9]. MTrPs are hyperirritable knots within discrete taut bands of skeletal muscle fibres that can alter sensorimotor and autonomic functions [10]. if MTrPs are formed in multiple muscle groups, they increase the number of sensitising substances that cause muscle spasms, localised or widespread pain, taut bands, autonomic dysfunction, hyperalgesia, and local twitch responses [11].
Electroacupuncture, gabapentin gel, and intraneural dex- amethasone injection are commonly used to desensitise SH in vivo [12]. Other treatments, such as transcutaneous electrical nerve stimulation (TENS), diadynamic current (DD), massage, and stretching exercises, were found to be effective for pain conditions when applied at adequate intensities. importantly, these interventions are not very effective in multilevel neural compression injuries in patients with SH [13-15]. Routine care treatments may not address all issues or produce immediate therapeutic benefits, especially in unique cases of SH with multiple sciatic nerve compression sites. Therefore, clinicians must emphasise the relaxation of tight muscles, deactivation of MTrPs, desensitisation of peripheral receptors and central neurons, increased flexibility of neural tissues, and blood circulation in the management of SH [16, 17]. Thus, further treatment options must be explored to achieve faster functional recovery in patients with SH.
Several studies have reported the effectiveness of deep dry needling (DDN) in various musculoskeletal disorders with peripheral and central sensitisation [18, 19]. in particular, one study demonstrated an increased blood supply in sciatic nerve areas after the application of dry needling, which may lead to desensitisation and regeneration of peripheral nerves [20]. dry needling is a safe and minimally invasive technique in which a thin solid acupuncture needle is inserted into specific areas of soft tissues to deactivate MTrPs, desensitise nociceptors, and improve muscle relaxation and blood circulation [21].
Neural mobilisation (NM) is a technique used in manipulative therapy to aid pain relief and restore function. it generally consists of techniques termed neural glides or neural flossing, which are more dynamic than neural stretching. The main objectives of NM are to achieve an overall balance in the nervous system and reduce nervous system sensitivity. Several studies have investigated the therapeutic efficacy of NM [16, 22], with a cross-sectional study using dynamic ultrasound imaging showing that different types of neurodynamic techniques resulted in differences in longitudinal sciatic nerve excursions [23].
The combined application of DDN for deactivating MTrPs and muscle relaxation and NM for increasing longitudinal sciatic nerve excursions and neural flexibility may provide better clinical outcomes in patients with SH. Therefore, this study aimed to evaluate the effectiveness of DDN combined with NM in improving clinical outcomes, such as pain, disability, kinesiophobia, and neural tissue flexibility, in patients diagnosed with SH.
Case description
Medical history
The two middle-aged patients, including a 56-year-old female and a 52-year-old male, were referred to physiotherapy with complaints of chronic widespread pain in the right lower limb. Both patients had a gradual onset of dull, diffused, intermittent lower back pain for several months and mild referred pain to the lower limb to the foot from month two. in the past few weeks, the patients experienced severe pain, pinprick pain sensations, hyperirritability to non-painful touch, and numbness over the territory of the sciatic nerve. in addition, they developed fear-avoidance behaviour during walking and other daily living activities [24]. The medical reports of the two patients indicated normal vital signs and levels of thyroid hormone and vitamin D within the reference range. Spinal magnetic resonance imaging (MRi) showed a mild intervertebral disc bulge in the female patient at L4-5 and L5-S1 and at L5-S1 in the male patient. Furthermore, medical reports indicated the absence of space-occupying lesions of the spine, such as tumours, abscesses, pelvic pathologies, hip arthritis, and other systemic diseases [24]. Since there were no contraindications or red flag signs identified during the medical examination, the patients were referred to physiotherapists for pain management and improved mobility functions.
Examination
No swelling, deformities, muscle atrophy, limb length discrepancy, postural deviations, or topical changes were observed. Superficial and deep tendon reflexes were normal on both sides, but muscle power could not be assessed since both patients were unwilling to move the affected lower limb due to severe pain [24].
Flat palpation of the piriformis muscle produced severe referred pain over the sacroiliac joint, gluteus, and hamstring muscles, which suggests the presence of MTrPs [10]. Similarly, palpation of the paraspinal, gluteus, hamstring, and deep calf muscles produced an excessive reaction to non-painful stimuli, which may be associated with peripheral and/or central sensitisation. The typical features of central sensitisation are excessive and abnormal psychological and physical reactions to non-painful stimuli, widespread pain, and paresthesias over the associated dermatome and myotome areas [25]. On further examination, the degrees of passive straight leg raise (SLR) were 20 and 25 in patients 1 (female) and 2 (male), respectively, alongside tightness of the piriformis, hamstring, and calf muscles.
Assessment of pain, disability and fear avoidance behaviour
The patients scored 10 points and nine points, respectively, on the numerical pain rating scale (NPRS). The NPRS is an 11-point scale ranging from 0 (“no pain”) to 10 (“the worst pain you can imagine”) and is a valid tool used to measure subjective experience of pain [26]. The Fear Avoidance Belief Questionnaire (FABQ) scores for work and physical activity were 100% and 88.09% in Patient 1 and 95.83% and 85.71% in Patient 2. The FABQ has been proven to be a reliable tool for assessing fear-avoidance behaviour [27]. The disability score on the Oswestry Low Back Pain Disability Questionnaire (OLBPDQ) was 88.9% for Patient 1 and 76% for Patient 2. The OLBPDQ is also a valid assessment tool for assessing disability caused by low back pain disorders [28]. Treatment outcomes are shown in Table 1.
Table 1
Clinical outcomes before and after treatment according to the NPRS, SLR, OLBPDQ, and FABQ work and physical activity scores
Intervention rationale
The subjective experience of severe widespread pain, low pain threshold, allodynia, and pinprick sensation in the sciatic nerve distribution, and MTrPs within the taut bands of paraspi- nal, piriformis, hamstring, and deep posterior leg muscles suggest that there is a possibility of multiple-level mechanical irritation of the sciatic nerve with sensitised nociceptors [1,2]. Thus, we hypothesised that desensitisation of nociceptors and relaxation of paraspinal, piriformis, hamstrings, and posterior tibial muscles using DDN and sciatic NM may relieve pain and associated functional disability faster.
interventions
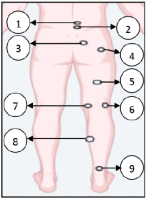
Written informed consent was obtained from the patients after providing detailed information about the potential therapeutic benefits and adverse effects of DDN and NM. Needling spots are shown in Figure 1.
Figure 1
A schematic representation of dry needling spots used in the patients: spots 1 and 2 -paraspinal muscles around 1 cm lateral to L4-5 and L5-S1 spinous process, spots 3 and 4 - proximal and distal piriformis muscle, spot 5 - biceps femoris, spot 6 - myotendi- nous junction of the biceps femoris, spot 7 - myotendinous junction of the medial hamstrings, spot 8 - flexor digitorum longus and tibialis posterior, spot 9 - myotendinous junction of the gastrosoleus muscles
Day one
Initially, spinal segmental DDN (0.25-mm thick x 40-mm length; SEIRIN® Corporation, Shizuoka, Japan) was administered. Dry needles (40 mm in length) were inserted at points 1 cm lateral to the spinous process line of the L3-S5 vertebrae, slightly inferior-medial, deep into the lumbar multifidi muscles. The presence of a dry needle was confirmed by touching the laminar surface of the vertebrae. Static needling was performed for 15 min to obtain maximum mecha- noreceptor stimulation and muscle relaxation. After removing the needle, the needle insertion sites were compressed with sterilised dry cotton for 10 s [16, 17]. After paraspinal dry needling, DDN was employed into the proximal and mid part of the piriformis muscle using 50 mm and 100 mm long dry needles (0.30 mm thick), respectively. DDN into the proximal part of the piriformis was employed in a perpendicular direction, and from the mid-point of the buttock, another long needle was inserted into the mid/distal part of the muscle with a 10-15° angle towards the MTrPs of the piriformis muscle. Several local twitch responses were elicited from the MTrPs by to-and-fro movements of the needle [29]. Both paraspinal and piriformis DDN were performed with the patients in the prone position.
Day two
With patients lying down, the MTrPs of the biceps femoris (prone), tibialis posterior, and flexor digitorum longus (supine) muscles were deactivated by eliciting a local twitch response from the MTrPs. Finally, static needling was employed for 10 min over the myotendinous junction of the hamstring and soleus muscles (prone) to achieve optimal muscle relaxation by Golgi tendon organ (GTO) stimulation [30].
Figure 1 shows a schematic representation of dry needling spots used in the patients.
Day three
After the dry needling procedure, sciatic NM was performed to create longitudinal tension in the sciatic nerve by increasing the SLR angle from 30° to 80°. Additional tension on the sciatic nerve was added to the hip adduction movement. On the third day, sciatic NM was initiated by performing a passive SLR from 30° to 60° within the patient’s pain tolerance, and the patient was instructed to actively perform alternate dor- siflexion and plantarflexion of the ankle for 10 repetitions to facilitate longitudinal nerve gliding [16, 17].
Days five and seven
On days five and seven, NM was performed at 70° and 80° of the passive SLR. At each position, 10 repetitions for each set and three sets of ankle movements were performed with 5 min rest between consecutive sets. The average total treatment time was approximately 30-40 min per session, and the whole treatment was administered for three sessions. The patient was instructed to continue NM exercises at home, with three sets of 10 repetitions per day, 3 days per week for 3 consecutive weeks [16]. The patient and their family members were asked to document all the information about the continuity of NM exercises in a given dairy.
Treatment outcomes
The data recorded before and after the treatment are presented in Table 1. Both patients achieved a significant reduction in pain, disability, and work/physical activity-related fear avoidance behaviour and improvements in SLR one week post-treatment (eighth day). At the one-month and six-month follow-ups, the patients completely recovered from pain and achieved a highly significant reduction in disability and fear- avoidance behaviours. Similarly, SLR was maintained above 80° in both patients after one and six months. Importantly, hyperalgesic symptoms such as pinprick sensation, supersensitivity, and allodynia over the sciatic nerve were absent at the one-month and six-month follow-up assessments.
A two-point change from the baseline pain score on the NPRS was set as the minimal clinically important difference in these patients after a week of intervention. We achieved more than an eight-point difference from the baseline score after one week of treatment. During the week of treatment, peripheral pain severity was significantly reduced, which also indicated a centralisation pattern of pain reduction. Further- more, the patient showed clinically significant improvements in disability, fear-avoidance behaviour and SLR. Follow-up outcomes at months one and six revealed that the patients were completely relieved from pain and could perform routine work and physical activity without any significant fear- avoidance behaviour.
Discussion
Sustained mechanical irritation of the sciatic nerve at multiple levels is responsible for widespread pain perception and altered movement patterns. Localised and widespread pain, fear of moving the affected leg, acute reduction of SLR, and protective muscle spasms in multiple muscle groups in the absence of any pelvic and systemic pathologies have been shown to be evidence of chronic sciatic pain [1,2]. As DDN and NM have been found to be effective in reducing peripheral and central sensitisation [19, 20], we employed these techniques to improve widespread pain, fear-avoidance behaviour, and lower limb function.
Dry needling has been suggested as a clinically effective intervention method, along with kinesiotaping and classic physiotherapy, to reduce the clinical manifestations of myofascial pain syndrome (MPS), such as pain and disability [21, 30]. The improvement obtained after two days of DDN is evidence of its effectiveness on MTrPs deactivation and desensitisation in patients with SH.
A systematic review of randomised controlled trials found that NM is effective in reducing pain and improving function in patients with various musculoskeletal conditions. Furthermore, the study suggests that NM is not superior to standard interventions or no treatment [22]. A prospective case series found that a standardised NM treatment strategy reduced neurogenic claudication related to degenerative lumbar spinal stenosis [32]. Another study also found that NM exercises ameliorated low back-related leg pain with peripheral nerve sensitisation [33]. These studies evaluated the effectiveness of either standalone DDN or NM on various clinical conditions associated with sciatic nerve dysfunctions. in this case study, applying DDN combined with NM achieved better clinical outcomes compared to the findings of previous studies.
This study indicates that DDN combined with NM can effectively modulate pain perception and muscle relaxation, even though mechanical overloading is present at multiple points of the sciatic nerve course. importantly, when applying just DDN to the paraspinal, piriformis, hamstring, and deep posterior compartment muscles during the first two days, the patient’s pain severity showed a centralisation pain pattern, which is attributed to the effectiveness of DDN. Therefore, the clinical outcomes obtained in these patients may help clinicians effectively treat similar clinical conditions in the healthcare field.
However, this case report had a few limitations. First, the sources of nerve compression at multiple levels were hypothetical and based on clinical manifestations, and the exact nerve compressions were not identified quantitatively through imaging or ultrasonographic methods. Second, we could not differentiate the hyperalgesic symptoms by determining if they were caused by chronic sciatic nerve compression by the adjacent musculoskeletal structures or the presence of MTrPs in multiple groups of muscles supplied by the sciatic nerve. Therefore, we recommend ultrasonographic evaluation to identify neural compression from adjacent musculoskeletal structures of the sciatic nerve in future studies.

