Introduction
Walking is one of the most fundamental activities in human daily life, requiring intricate coordination between various sensory systems and the neuromuscular system for balance and spatial orientation [1]. Postural control and balance are critical not only during walking but also during standing, running, and other daily activities [2]. Assessing balance performance using force plates provides insights into postural control effectiveness, which is crucial for preventing falls in the elderly, rehabilitating neurological patients, and optimising athletic performance [3].
The measurement of ground reaction forces (GRF) using force plates is particularly relevant for understanding movement patterns and their implications across diverse populations, including children, individuals with cerebral palsy, the elderly, neurological patients, and athletes [4]. Analysing kinetic and kinematic parameters, along with GRF, centre of pressure (CoP), and plantar pressure distribution (PPd), yields valuable insights into movement patterns and aids in designing tailored interventions and exercise programs [3].
The integration of force plate technology into various research fields, from biomechanics to clinical rehabilitation, has revolutionised our understanding of human locomotion and postural control [5]. By providing precise data on parameters such as CoP and moment patterns, force plates facilitate meticulous analyses of movement dynamics and treatment efficacy [6]. As technology advances, force plate systems are becoming more accessible and cost-effective, making them indispensable assets in both research and practical applications [7]. in recent years, force plates have been increasingly utilised in innovative experiments and applications. For example, researchers have explored the use of force plates to study the effects of different footwear on gait patterns and postural stability [8]. Additionally, force plates have been integrated into virtual reality systems to create immersive rehabilitation environments for patients recovering from injuries or surgeries [9].
Furthermore, advancements in machine learning and artificial intelligence have enabled the development of sophisticated algorithms for analysing force plate data. These algorithms can automatically detect subtle changes in movement patterns and provide real-time feedback to clinicians and patients during rehabilitation sessions [10].
However, current force plates are often expensive, cumbersome to operate, and lack mobility [11]. There is a growing demand for low-cost and portable force plates to enable effective posture and gait assessments in various settings, including hospitals and research laboratories. Researchers are actively working towards developing affordable and user-friendly force plate solutions to address these challenges and further enhance the accessibility and applicability of force plate technology.
Force plates have emerged as indispensable tools in understanding human movement and postural control across diverse populations and research domains. Their ability to provide precise data on movement parameters contributes to the development of tailored interventions and rehabilitation strategies, ultimately improving human health and performance. Efforts to make force plate technology more affordable and portable will further broaden its impact in research and clinical practice, paving the way for continued advancements in movement science and healthcare. The main aim of this research is to evaluate human posture by utilising a low-cost force plate. This study emphasises the potential applications of this approach in assessing key postural parameters, including GRF, CoP, and PPd.
Subjects and methods
Construction of a hardware instrument and software development
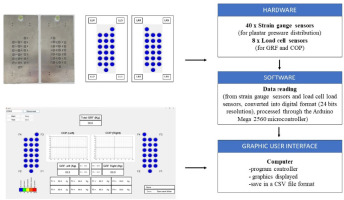
Testing equipment includes aluminium sheets sized 250 × 500 × 6 mm, strain gauges, single-axis load cells, micro-controllers, signal amplification modules, and a computer (Figure 1).
Participants
This study based our approach on a published article [2] which included only 4 participants. However, to enhance the reliability of our experimental results, we expanded our sample size to 15 participants through random selection.
Experiment variables
Experimental procedure
Static standing test
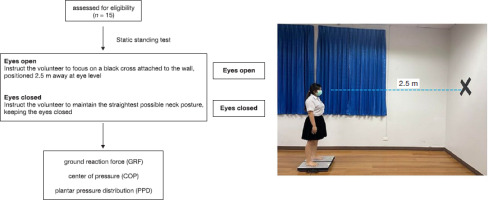
This test was conducted under two conditions: with eyes open and with eyes closed for 30 s.
Eyes open: Volunteer instructed to focus on a black cross attached to the wall, positioned 2.5 m away at eye level.
Eyes closed: Volunteer instructed to maintain the straightest possible neck posture, keeping the eyes closed.
Perform the test three times for each condition. After each standing trial, the volunteer was asked to sit and rest for 1 min before proceeding to the next trial.
Volunteer was to stand upright, barefoot, maintaining the most stable posture with arms placed naturally alongside the body without swaying or moving.
Record the time the volunteer stands for 30 s and document the results.
Statistical analysis
All statistical analyses for this research will be conducted using SPSS Statistical Software (SPSS version 23). The data collected for this study, encompassing general information such as age, height, weight, and body mass index, will be analysed in terms of mean values and standard deviations. The dependent variables analysed in this study were used to describe the volunteer’s postural behaviour. This included the calculation of the mean medial-lateral (ML) amplitude (cm) of the CoP and the calculation of GRF by the load on the left/ right foot (kg). Additionally, PPd was evaluated by the foot’s pressure on the position of the strain gauge.
Results
Characteristics and traits of research participants
The number of volunteer participants for this research was comprised of individuals in good health with ages ranging from 18 to 25 years, totalling 15 individuals. The average age of the volunteers was 21.67 ± 0.90 years, with an average height of 161.00 ± 0.07 cm. The average weight was 59.42 ± 14.06 kg, and the average body mass index was 22.83 ± 4.65 kg/m2. The gender distribution shows 27% male participants (4 individuals) and 73% female participants (11 individuals). All participants exhibit right-foot dominance. The general characteristics of these volunteers are summarised in Table 1.
Study results of the developed postural assessment tool in healthy volunteers
The examination of the postural assessment tool was conducted on 15 healthy volunteers. Participants stood on a force platform for 30 s with both eyes open and closed, and this was repeated three times. The study focused on analysing the GRF, CoP, and PPd.
Ground reaction forces (GRF)
From the study results of the GRF during the eyes-open condition in the 15 volunteers, it was observed that there was more load on the left foot in 8 individuals, constituting 53.33%, and on the right foot in 7 individuals, constituting 46.67%.
Regarding the GRF during the eyes-closed condition, the study found that there was more load on the left foot in 9 individuals, constituting 60%, and on the right foot in 6 individuals, constituting 40%, as shown in Table 2.
Centre of pressure (CoP)
The study of the CoP during the eyes-open condition revealed lateral deviations to the left, ranging from 0.00 to 1.75 cm, and the right, ranging from 0.00 to 3.00 cm. during the eyes-closed condition, lateral deviations to the left were observed in the range of 0.26 to 2.75 cm and the right in the range of 0.00 to 3.50 cm, as illustrated in Table 3.
Table 3
Centre of pressure during eyes-open and eyes-closed conditions
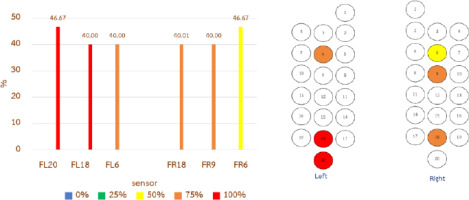
Plantar pressure distribution (PPd)
The PPd parameter utilises a colour-coded distribution from 40 × strain gauge sensors to illustrate variations in force levels across different areas, providing pressure distribution patterns on the left foot at positions 1–20 and the PPd parameter on the right foot (FR) at positions 1–20. The study of PPd on the left foot during the eyes-open condition revealed the three positions with the highest load as follows: Position FL20, with 100% load (46.67%); Position FL18, with 100% weight-bearing (40.00%); and Position FL6, with 75% load (40.00%). on the right foot during the eyes-open condition, the three positions with the highest load were: Position FL18, with 75% load (40.01%); Position FL9, with 75% load (40%); and Position FL6, with 50% load (46.67%), as shown in Figure 3.
Figure 3
Plantar pressure distribution (PPd) on the left and right foot during the eyes-open condition
Regarding PPd on the left foot during the eyes-closed condition, the top three load positions were: Position FL20, with 100% load (60%); Position FL18, with 100% load (46.66%); and Position FL6, with 75% load (53.33%). on the right foot during the eyes-closed condition, the three positions with the highest load were: Position FL18, with 100% load (33.33%); Position FL9, with 75% load (40%); and Position FL6, with 50% load (53.33%), as depicted in Figure 4.
Discussion
A study on GRF during the eyes-open condition revealed that there was a greater weight distribution on the left foot by 8 individuals, accounting for 53.33%, and on the right foot by 7 individuals, constituting 46.64%. during the eyes-closed condition, a weight distribution on the left foot by 9 individuals, constituting 60%, and on the right foot by 6 individuals, accounting for 40%, was observed. These findings align with a previous study that examined weight distribution in women, indicating a 52.33% weight on the left foot, which was higher than the 47.67% on the right foot. This is attributed to the body’s postural control mechanisms, involving the central nervous system, sensory perception, and musculoskeletal system [12]. When various types of sensory receptors are stimulated, the brain’s motion control areas analyse the data and determine appropriate movement patterns or weight distribution for maintaining balance [13]. The results of this assessment demonstrate postural control, a parameter indicating abnormalities in body posture, which can contribute to injury prevention [14]. Understanding postural control may help identify issues in patients or the elderly, such as those with neurological disorders or muscle weakness, as seen in Parkinson’s disease patients. it allows for the assessment of postural control through GRF values [15, 16]. in summary, previous studies emphasise the significance of GRF in assessing stability in postural control [17].
From the study of the CoP, it was observed that during the eyes-open condition, the CoP leaned to the left by a distance of 0.00–1.75 cm and to the right by a distance of 0.00– 3.00 cm. during the eyes-closed condition, the CoP leaned to the left by a distance of 0.26–2.75 cm and to the right by a distance of 0.00–3.50 cm. Automatic postural reactions, the body’s response to maintain balance, involve muscle activity and minimal energy expenditure. When disturbances occur, causing the centre of mass (CoM) to deviate from the base of support (BoS), automatic postural reactions quickly restore balance by pulling the CoP back into the new BoS, preventing falls [18]. The length of the CoP deviation reflects the maintenance of body balance while standing. A smaller deviation indicates greater stability [19]. The body’s upright posture is influenced by the gravitational force, resulting in acceleration or deceleration of the CoM. The CoP is directly related to the CoM, emphasising the importance of the BoS. The BoS is the area where the CoP can move to maintain body balance, swiftly shifting the CoP to prevent the CoM from moving outside the BoS [20]. The speed and distance of CoP movement significantly affect dynamic balance control during motion. Furthermore, studies on body balance across various age groups show that the average CoP distance is higher in older individuals than in younger ones [19, 21]. Analysis of the CoP can be used to evaluate clinical conditions such as motor recovery, sensory reception, and cognitive understanding [11]. By examining the CoP movement in the anterior-posterior (AP) and ML directions, which indicate the ability to control posture, clinicians can assess the patient’s ability to maintain balance [22]. Additionally, the distance between the highest and lowest points of the CoP in the AP and ML directions is crucial. A greater distance suggests poor postural control. The CoP distance is a reliable parameter used to evaluate postural stability, especially in the ML direction, often employed in assessing individuals with abnormal movement control [23]. Several studies have shown that when assessing postural sway, attention should be given to the CoP excursion [24–29]. This aligns with research by Golriz et al. [30], stating that the speed and distance of the CoP are reliable parameters for evaluating postural control.
From the study of PPd, it was observed that the left foot’s pressure distribution during the eyes-open condition had the highest weight in three positions. These positions were the toes (FL20), with a weight of 100%, accounting for 46.67%, the front of the foot (FL18), with a weight of 100%, accounting for 40%, and the midfoot front part (FL6) with a weight of 75%, accounting for 40%. The PPd of the right foot during the eyes-open condition in the areas with the highest weight had the following three positions: the front of the foot (FL18) with a weight of 75%, accounting for 40.01%, the midfoot sole (FL9) with a weight of 75%, accounting for 40%, and the midfoot front part (FL6) with a weight of 50%, accounting for 46.67%. in the study of the PPd of the left foot during the eyes-closed condition in the areas with the highest weight, the top three positions were the toes (FL20) with a weight of 100%, accounting for 60%, the front of the foot (FL18) with a weight of 100%, accounting for 46.66%, and the midfoot front part (FL6) with a weight of 75%, accounting for 53.33%. The PPd of the right foot during the eyes-closed condition in the areas with the highest weight had the top three positions as follows: the front of the foot (FL18) with a weight of 100%, accounting for 33.33%, the midfoot sole (FL9) with a weight of 75%, accounting for 40%, and the midfoot front part (FL6) with a weight of 50%, accounting for 53.33%. These findings are consistent with the research of Ang [31], who studied PPd while standing on flat and inclined surfaces in healthy individuals aged 19–24 years. The study placed sensors at six positions on the foot, including the big toe, inner side of the forefoot, mid-forefoot, outer side of the forefoot, mid-midfoot, and the heel. The results showed that the highest PPd occurred at the forefoot, followed by the mid-fore-foot. As the surface incline increased, there were changes in weight distribution towards the forefoot, indicating variations in the PPd with different foot positions. Furthermore, investigated foot weight distribution in healthy females, revealed a weight ratio of 1:2 between the forefoot and the mid-foot to heel. The greater pressure on the forefoot is attributed to the line of gravity, starting from the body’s CoM and descending through the forefoot before spreading to the front part of the foot [32]. The force or weight applied to the forefoot comes from the human body’s part that extends furthest in the lower limb, which is the forefoot itself [33]. Currently, there is a study on the distribution of foot pressure that can serve as an indicator or predictor of foot-related issues. Changes or abnormalities in the distribution of pressure on the feet may result from various factors such as weight, gender, foot structure, or even individual posture and walking characteristics. The assessment of foot pressure distribution can be conducted while standing, walking, or engaging in various activities using sensors on the soles of the feet or a force plate to assess abnormalities or potential diseases. This is crucial as the feet are the first lower body structure that experiences force, transmitting it to the knees, hips, and the spine. Problems can be identified during both standing and walking, impacting the daily activities of humans significantly. The majority of human daily life involves standing and walking, where the feet act as the force receptors from the ground. The irregular forces generated can lead to stress, potentially causing problems with the foot’s structure. This may result in future issues such as foot injuries and other structural problems [34]. Previous studies have shown that low-cost force plates offer accurate measurements comparable to standard ones, making them suitable for biomechanics and sports research. Portable wireless force platforms like K-deltas showed high agreement with standard plates for various tests [35, 36]. Low-cost portable force platforms proved reliable for measuring weight, static positioning, and jumping [37]. Studies indicate that low-cost force plates can offer accurate and accessible force measurements for biomechanics applications like expensive, standard ones.
Limitations
The developed tool cannot display the speed of body sway while standing. our study did not examine foot characteristics because the pressure or distribution of pressure on the feet may vary abnormally. This research utilised data from all developed tools. other scientific instruments may have been used to confirm that the results are consistent.
As our equipment remains in the prototype phase, it has been designed to address our research goals, particularly focusing on parameters like GRF, CoP, and PPd. However, we’re facing a problem because we don’t have access to different types of standard force plates for comparison. in the future, we hope to get standard force plates to make our results more reliable.
Conclusions
The research conducted in this study aims to investigate the development of prototype tools for the assessment of posture, with the specific objective of enhancing ease of use, facilitating convenient installation, and ensuring precise assessment capabilities. These tools are designed to measure various parameters, including GRF, CoP of the foot, and PPd. The intended application of these developed tools encompasses posture assessment in elderly populations to mitigate the risk of falls, a predominant cause of injuries among this demographic. Moreover, they serve as valuable screening instruments for individuals presenting with diverse posture-related concerns, with the acquired data informing subsequent assessment, treatment planning, and monitoring processes. Notably, these tools are characterised by their user-friendly nature, straightforward installation procedures, and intuitive operation, thereby enabling streamlined and expedited assessment procedures. Furthermore, their versatility extends beyond laboratory or hospital settings, rendering them particularly conducive to the assessment of elderly individuals or community patients. Additionally, their utilisation has the potential to mitigate travel-related expenses associated with hospital visits for treatment monitoring, thereby optimising resource allocation and alleviating the workload of medical personnel.
Clinical application
Postural control refers to the body’s ability to manage and maintain the centre of gravity (CoG) within the BoS, ensuring balance in both stationary and moving positions [35]. Achieving balance and controlling body posture rely on the coordinated functioning of various body systems [18]. Any abnormalities may compromise balance and postural control, increasing the risk of falls. Assessing the risk of falls can help mitigate injury or fatality risks. one useful tool for fall risk assessment is the force plate. By examining the CoP values, which indicate body sway related to fall risk, deviations from the centre or outside the BoS can increase the likelihood of falling.