Introduction
The piriformis syndrome is a result of prolonged sitting. Many women spend long periods sitting down, whether at work or home. This syndrome could be attributed to the rapid routine of contemporary daily lifestyles. Piriformis syndrome may cause incapacitating lower back or buttock pain that ranges from mild to severe. A male-to-female ratio of 1:6 has been found for cases of piriformis syndrome, which usually affects middle-aged female adults. if untreated, it can have a negative effect on a woman’s quality of life [1–3]. Piriformis syndrome is a type of peripheral neuropathy that causes irritation and strangulation of the sciatic nerve. it is responsible for 0.3% to 6% of all occurrences of sciatica and low back pain. There are approximately 2.4 million cases of piriformis syndrome worldwide per year [2].
Piriformis syndrome has primary and secondary causes. Primary piriformis syndrome, which accounts for 15% of cases, is connected to the anatomical positioning of the piriformis muscle and sciatic nerve. Secondary piriformis syndrome is caused by recurring precipitating factors such as microtrauma, macrotrauma, and local ischemia [2]. Trauma to the gluteus and pelvic regions is a risk factor that is frequently considered an inducer of piriformis syndrome. Secondary piriformis syndrome is more common in skiers, tennis players, and long-distance bikers [3]. Among the most common causes of piriformis syndrome are myofascial trigger points (TPs) that develop over the piriformis muscle as a result of changing or increased muscle demands [4]. Patients with active TPs may exhibit any of the following symptoms during a physical examination: local discomfort, referred pain, replication of pain with compression on the muscle, and an evoked local twitch reaction with snapping palpation. Also, many have decreased range of motion (RoM), muscle weakness, muscle stiffness, and a general decline in function in addition to discomfort [5].
Numerous therapies have been created to address the aforementioned problems by reducing active TPs. The treatment solutions include physical therapy, muscle relaxants, nonsteroidal anti-inflammatory drugs, and brief rest for no more than 48 hours. For some cases, piriformis muscle injections with steroids may be beneficial [6]. Physiotherapy management for piriformis syndrome includes stretching the piriformis muscle as well as utilising heat and ultrasound therapy. Moreover, manual therapy methods like the active release technique (ART), muscle energy technique; strain/counter-stain, spray and stretch, transverse friction massage, and ischemic pressure technique (iPT) to treat the active piriformis TPs [7]. iPT and ART techniques increase oxygen consumption and nutrient intake by the muscle tissue [8].
iPT is a non-invasive procedure that involves applying perpendicular pressure across the TP for 90 s in an attempt to modify the texture of the area. in the form of reactive hyper-aemia or as a result of the spinal reflex mechanism, the benefits of post-compression blood supply provide all the necessary cellular energy requirements, nourishment, and oxygen. These techniques increase the active RoM while enhancing muscle length and flexibility to combat the effects of energy crises [7, 9–13]. in the available literature, five similar studies have investigated the effect of iPT in patients with active TPs: Mujawar et al. [7] measured hip internal rotation RoM, the oswestry disability Scale (odS), and the visual analogue scale (VAS) after iPT in patients with piriformis tightness. Yousef et al. [10] measured neck rotation and lateral flexion after releasing cervical TPs. Gemmel et al. [11] and Suresh et al. [12] measured the pressure pain threshold (PPT), RoM, and the level of disability in the upper extremity by Neck disability index (Ndi) after releasing the active TPs in the upper fibres of the trapezius. Morask et al. [13] evaluated the physiological changes that occur at the active TPs following iPT in patients with chronic headaches. These studies found that iPT is beneficial in the treatment of active TPs. After iPT, the affected muscle’s discomfort decreases and its RoM and functions are increased [10].
ART is a type of manual therapy used for restoring soft tissue function. This non-invasive soft tissue treatment method finds and dissolves adhesions and scar tissue that contribute to physical dysfunctions such as pain, stiffness, weakness, and numbness. it can also be used to treat muscles, tendons, ligaments, fascia, nerve tissues and active TPs [14–16]. Similar studies discussed ART’s impact on active TPs and pain in the previous five studies: Robb et al. [14] reported improvements in muscle PPT when ART was added to conventional physical therapy treatment of patients with an adductor strain. Also, Tak et al. [15] found improvements in the score of VAS and PPT in participants with active TPs in the lower back. in addition, George et al. [16] assessed the hamstring muscle after releasing its active TPs and reported improvements in VAS and knee extension after having ART. Mujawar et al. [7] measured hip internal rotation, odS, and VAS following ART in participants with piriformis syndrome. Also, Nambiraga et al. [17] discovered improved VAS changes, lower extremity functional ability, and PPT after adopting ART in the treatment of participants with piriformis syndrome with active TPs.
Comparing iPT and ART effects on women with active TP and piriformis syndrome was the study’s main objective. iPT was examined for the first time to determine which technique is better to improve one’s quality of life. iPT and ART are both non-invasive, soft tissue, manual techniques used to treat active TPs, but which one is more effective? Therefore, the present study intended to compare the effect of iPT versus ART on female patients with piriformis syndrome. This includes measuring the degree of pain, RoM, and lower extremity function in female participants. Comparing the outcomes of the two techniques can help physical therapists in their decision-making in treating and improving the overall outcome of patients with active piriformis TPs.
Subjects and methods
This study was conducted from November 2020 to March 2022 at the outpatient clinic of damietta Specialized Hospital, Egypt. Participants were diagnosed and referred with chronic piriformis syndrome for more than 3 months with active piriformis TPs by the orthopaedic doctor. All subjects were checked for the presence of active TPs in the researched muscle. A clinical diagnosis of active TPs must meet at least one of the three secondary criteria, in addition to the five primary criteria, according to Simons’ diagnostic guidelines. The primary criteria were as follows: local discomfort, an anticipated pattern of referred pain, tactile taut bands, restricted hip motion, and a tender area along the taut band. The secondary criteria included a local twitch reaction, pain that was relieved by stretching, and discomfort that was reproduced by pressure on the nodule [5].
Study design
The current study is a single-blinded, randomised, controlled trial. The study followed the CoNSoRT guidelines [18].
Participants
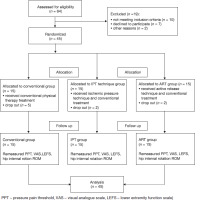
Sixty-four females were randomly enrolled by an online random generator (https://www.random.org/integers/) by the second author, who was not involved in the treatment or assessment. during the first screening session, the study excluded nineteen participants as they were ineligible because of a recent lower extremity fracture, inflammatory joint diseases, soft tissue injuries, lumber canal stricture, lumber disc herniation, lumber spondylosis, or utilising any type of pain-killer or inflammatory medications over the last 72 hours. All participants were screened for the existence of piriformis syndrome by the fourth author. diagnostic criteria were as follows, gluteal pain, predicted pattern of active TPs of piriformis syndrome, referred pain, and a tender spot at one point along the palpable taut band. in addition, they showed a positive flexion adduction internal rotation (FAiR) test, the Freiberg test, and the pace abduction test [19]. Forty-five participants aged 25–40 years met the diagnostic criteria, and in the end, 9 participants dropped out, as shown in Figure 1.
Randomisation
According to the CoNSoRT, the chit method of fundamental randomisation was adopted to evenly divide the participants into three groups by the third author who was not involved in the treatment or assessment. in total, 45 little chits were placed within a box that each participant had access to. The first fifteen were assigned to the conventional group, the second fifteen to the iPT group, and the third fifteen to the ART group. The numbers were written on chits. There was the same number of participants in each of the three study categories. The three groups received conventional physical therapy treatment protocols: the conventional group received physical therapy treatment only. The iPT group received physical therapy and iPT. The ART group received physical therapy treatment and ART. The treatments were performed by the first author.
Sample size calculation
Sample size calculations were computed with 80% power, a significance level of 0.05, and a VAS difference between the three groups of 0.55 (effect size, ES). The sample size was calculated to be 12 people per group [20]. A pilot study with 5 participants in each group served as the basis for the estimated impact size. Each group required at least 15 participants, assuming a 20% loss to follow-up [20]. The sample size calculations were carried out using G*Power statistical software (version 3.1.9.2; Universität Kiel, Germany) and resulted in 45 participants.
Outcome measurements
The study was adopted for the measurement of pain intensity levels, hip internal rotation, function disability levels, and PPT. A detailed evaluation was done before initiating the intervention and after 12 sessions of physical therapy.
The pain intensity level was measured by VAS. This graphic rating system is used to keep track of various pain intensity levels and is frequently regarded as a trustworthy way to gauge pain intensity levels. on the VAS, which has a 10-cm length, zero means no pain, and the patient’s worst pain experience equals ten. on the line representing the level of pain, each participant was asked to score themselves before and after the physical therapy intervention. it is sufficiently valid and reliable [21].
The hip internal rotation was measured using a universal goniometer. The simplicity of measuring hip internal rotation, the ability to measure joint angles, and it’s inexpensive are advantages of goniometry. Goniometric testing is a precise and dependable method to track changes in hip RoM. Goniometry is a reliable and valid measurement method [22]. during the test, the participants were asked to sit with their hips and knees flexed to 90 degrees. The distal arm of the goniometer was placed on the vertical line from the patella to the floor, with the proximal arm on the midline of the lower leg (the line joining the medial and lateral malleoli to the patella’s centre) [23].
Lower extremity functional levels were measured by the Arabic version of LEFS [23]. it is a very helpful tool used by researchers and others who assess illnesses to determine their level of functional limitation. The researchers’ excellent test-retest reliability and Pearson correlation coefficient value greater than 0.7 were observed with the LEFS scores, which were extremely responsive. This useful tool for self-assessment is reliable and valid. Before initiating the study and again at the end of the study after completion of the physical therapy treatment program, the participant was asked to mark the current level of disability on the LEFS items. A total is calculated by adding the scores for individual items. The differences between these two values were identified prior to and following physical therapy treatment [24, 25].
PPT was measured by the baseline pressure algometer, model B153250122, made by Fabrication Enterprises in White Plains, New York. A typical flat, circular probe is applied to measure the level of discomfort at the Piriformis TPs. it appears to be a reliable and valid technique for identifying discomfort [26]. Acupuncture point GB30, which is situated in the middle of the muscular belly, is the most active TP in the piriformis in a vertical direction. The participants were lying face down, their affected leg in flexion and abduction of the hip. They were supported by the therapist’s thigh [27]. The algometer probe tip was applied to the central area of the muscle belly. Each female was told to raise her hand or say “ouch” when feeling any sort of discomfort. The requisite pressure was provided to the algometer by firmly pressing it downward [28].
Procedures
The three groups received conventional physical therapy treatment protocols by the first author who was not involved in assessment or randomisation: the conventional group received conventional physical therapy treatment only. The iPT group obtained conventional physical therapy treatment and iPT. The ART group received conventional physical therapy treatment and ART.
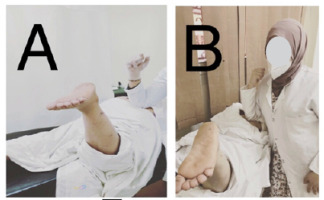
The treatment protocol encompassed six weeks with two sessions a week. Twelve sessions were completed. Each session lasted for about 40 to 50 min [29]. The three groups received the hot pack technique while lying on their backs. Hot packs (PVC pad and Fleece cover, 220–240V, 50 Hz, 60 W) were placed on the gluteal area and the lateral side of the thigh for 20 min [30]. Then, using a symmetrical biphasic pulse current waveform with a 100 Hz frequency and 200 ms pulse length, TENS (Multi current Gymna unify, model CE0339, code 65245) treatment was provided for 20 min. The level of stimulation was set at 80% of the pain threshold, according to each participant. one electrode was placed at the ischial tuberosity and the other at the greater trochanter while the patient lay in the prone position [31]. The stretching exercises were performed with the participants lying on their backs with their knees bent and their feet flat on the ground to achieve a static stretching mode. The right leg’s ankle was placed on the left leg’s knee. The left thigh was pulled toward the chest while holding the stretch for 30 s. Repeated three times with a 30-second break [32, 33]. iPT, as shown in Figure 2, participants were asked to lie on their stomachs near the edge of the table. Standing parallel to the participant, the therapist was by the patient’s side. The therapist gently pressed the piriformis active TPs, located in the muscle belly of the piriformis at mid-buttock, using the elbow. The piriformis muscle was relaxed by externally rotating the leg. The pressure was raised to get to the piriformis level. With a feeling of tension released under the finger used for palpation, the pressure was maintained. in some cases, the participant’s pain significantly decreased. At this point, the therapist could reach the next barrier until pressure on the piriformis TPs provoked only a little discomfort without pain after 90 s [12, 17, 34].
Figure 2
Ischemic pressure technique: (A) piriformis active TPs located at mid-buttock, (B) therapist pressed the active TPs using the elbow, (C) relaxing piriformis by externally rotating the leg

ART, as postulated in Figure 3, the participants were lying face down at the edge of the table with their knees flexed to 90 degrees. The therapist stood next to the subject and placed an elbow on the piriformis TPs in the muscular belly of the piriformis at mid-buttock [7]. After applying deep pressure over the TPs, the participant was asked to voluntarily take the muscle into the stretched position by internally rotating the thigh to lengthen the piriformis. By doing this, the adhesions were released, and the soft tissues’ normal flexibility, texture, and function were restored [14].
Statistical analysis
Using SPSS Version 28, data management and statistical analysis were done (iBM, Armonk, New York, United States). To ascertain the normality of quantitative data, the Shapiro– Wilk test and techniques for direct data visualisation were applied. Numerical data were reported as means and standard deviations, or medians and ranges, according to normality testing results. A one-way ANoVA test was used to compare the demographic data as it was normally distributed. Kruskal–
Wallis tests were employed as the VAS, LEFS, RoM, and PPT, were not normally distributed to compare the results between study groups. Mann–Whitney U analysis was carried out in the event of overall significance, and each post hoc analysis was corrected for multiple comparisons. There are two sides to every single statistical test. Significant results were defined as p-values of 0.05 or less.
Results
Demographic characteristics
As presented in Table 1, a one-way ANoVA test showed no statistically significant variances between any of the three study groups’ age, height, weight, or BMi (p > 0.05). Also, there was no statistically significant variance between the three groups in VAS, RoM, LEFS, and PPT.
Table 1
Demographic characteristics of participants
Statistical analysis of all outcome measures
Among group analysis
The Kruskal–Wallis test results indicated that there was no statistically significant difference between the three groups at the baseline measurements for the dependent variables (VAS, hip internal rotation RoM, lower extremity functional scale, and PPT). on the other hand, as shown in Table 2, there was a significant difference between the groups in the post-treatment comparison for all variables that were measured.
Table 2
Pre- and post-treatment statistical analyses of all outcome measures between the groups
Within-group analysis
All measured variables in all study groups showed a statistically significant difference between pre- and post-treatment according to the Wilcoxon signed-rank test, as shown in Table 2. The average effect of the intervention was estimated using Cohen’s d to compute ESs. According to the Cohen method, post-treatment d in VAS was 0.33, denoting a medium effect with significant clinical importance; d in hip internal rotation RoM was 0.173, denoting a minimal effect with minimal clinical importance; d in LEFS was 0.087, denoting a minimal effect with minimal clinical importance; and d in PPT was 0.200, denoting small effect with minimal clinical importance.
Multiple pairwise comparisons
Multiple comparisons between groups were conducted using post hoc analysis and the Bonferroni correction. The test resulted in crystal-clear variances favouring the iPT group between conventional and iPT groups. Additionally, there was a statistically significant difference in favour of the ART group between conventional and ART groups. Even though there was no significant difference between iPT and ART groups, as shown in Table 3. data missing from measurements taken later, after treatment, were accounted for using an intention-to-treat analysis with multiple imputations.
Table 3
Post-treatment comparisons between groups
Discussion
The current study was carried out to compare the effects of ART versus iPT on pain intensity levels, hip internal rotation RoM, function disability levels, and PPT in females with piriformis syndrome. The current study concluded that both ART and iPT were beneficial in treating piriformis syndrome in terms of PPT, VAS, LEFS, and hip internal rotation. However, greater percentages of improvements were identified in the ART group.
The results of this study showed statistically significant differences between pre- and post-treatment in pain, function levels, and hip internal rotation RoM within both groups (B and C). The average ES of the intervention was estimated, the post-treatment ES for VAS was 0.33, denoting a medium effect with significant clinical importance; ES in hip internal rotation RoM was 0.173, denoting a minimal effect with minimal clinical importance; ES in LEFS was 0.087, denoting a minimal effect with minimal clinical importance; and ES for PPT was 0.200, denoting a small effect with minimal clinical importance. Post-treatment, there was a statistically significant difference between groups in terms of pain, function, and hip internal rotation, but there were no statistically significant differences between iPT and ART post-treatment. in this study, conventional physical therapy had a significant impact, which may be attributed to the hot packs’ ability to dilate the blood vessel wall, permitting more nutrients, oxygen, and blood to flow, which promotes recovery and relaxes the muscle fibres, which reduces muscle tension and suppresses pain while simultaneously exerting pressure on the piriformis muscle and blocking the pain impulses [32, 35, 36]. TENS reduces muscular tension and raises the pain threshold for pressure. Firstly, a decrease in motor neuron activity and a drop in sensitivity of muscle spindles are caused by a decrease in sensory system input brought on by TENS’ pain-inhibiting actions. due to the regulation of the hyperactive muscular tone, the muscles’ viscoelasticity was reduced, and RoM improved [31]. it has been proven that piriformis muscle stretching procedures speed up recovery from piriformis muscle syndrome. Stretching improves physical performance, increases flexibility, lowers the risk of injury, and reduces muscular soreness [31, 32].
Nakano’s meta-analysis [36] of 12 randomised clinical studies is in line with this study. it has been found that stretching alone has less effect than therapies combining stretching and hot packs. Also, it has been claimed that thermal treatment reduced the viscosity of connective tissue and viscoelasticity at higher temperatures while increasing collagen extensibility [36]. Also, a study by Hou et al. [9] found that a variety of physical interventions and therapeutic exercises had an effect on releasing TPs. Five therapeutic combinations, including TENS, iPT, stretching, interferential current, and myofascial release approaches combined with hot packs and active RoM exercises, were evaluated and contrasted [17]. in the current study, iPT relieves TPs by extending sarcomeres while lessening their height in the muscle fibres. The TP’s dialysate glucose concentration rose twenty minutes after the TPs were released. The area’s blood flow was enhanced, respectively [11–15]. According to this theory, the TP nodule was released, nourishing blood flow to the tissue occurred, and improved oxygen supply and substrate perfusion helped skeletal muscle meet the energy needed for equilibrium recovery. Therefore, it is possible to increase the joints’ flexibility and RoM. The subsequent muscular contractions could trigger a large return of blood [9]. The disadvantages of iPT are hand overload and an exhausting technique [12].
Gemmell et al. [11], in agreement with the current study, undertook a randomised, single-blind, placebo-controlled investigation. it has been concluded that iPT has an effect in lowering pain and releasing TPs. Moreover, in a biological study by Moraska et al. [13] to measure the physiological changes within active TPs during iPT, the interstitial fluid at the TPs was continuously collected both before and after the intervention (iPT). it has been determined that modifications to cellular metabolism happen quickly and stay elevated within active TPs after iPT. in the current study, the effect of ART may be attributed to releasing the TPs by locating and dissolving the scar tissue and adhesions that result in pain, weakness, stiffness, numbness, and physical dysfunction. Tissues attempt to repair themselves when they are damaged. They are finished by immune responses. The immune system fights against infection and heals the wound. ART restores all soft tissue movement and frees nerves that have been imprisoned [37–39]. The manual touch of the therapist during ART stimulates the iV receptors, and their activation stimulates the supraspinal pathway, which leads to the production of the inhibitory neurotransmitter, which in turn lowers muscle tone and disrupts the pain-spasm-pain loop. The transfer of pain perception via the suprathalamic route is lowered because the reduction of muscular tone improves blood circulation and flushes out the inflammatory substances stored in the spasmodic muscle [39]. The disadvantages of ART are hand overload and it’s a painful technique [38]. in accordance with Nambiraja et al. [17] who investigated the impact of ART on piriformis syndrome pain relief and in agreement with the current study, ART has beneficial benefits for pain management. Additionally, Kage et al. [37] reached the same conclusion about ART; the procedure increases the RoM while lowering the problem of discomfort. it is employed to treat recent wounds, functional fixation damage, and repetitive strain injuries brought on by prolonged poor posture. The removal of soft tissue adhesions caused by scar tissue, which causes discomfort, spasms, paralysis, and tingling, is another benefit of ART [37]. Furthermore, Nambiraja et al. [17] showed that ART may have some improvements over other groups in a pilot study evaluating the effects of stretching, iPT, and ART on piriformis syndrome cases. in contrast to the current study, Mujawar et al. [7] concluded that iPT has a larger effect in treating piriformis tightness than stretching. However, stretching had a lesser effect than iPT and ART [7]. Moreover, dey and Pal [38] found that both ART and iPT reduce discomfort and disablement and improve joint RoM. According to this study, both ART and iPT reduce piriformis TPs, reduce gluteal discomfort, and increase hip internal rotation.
According to the current study, there was no statistical difference between both groups, this may be attributed to both non-invasive manual techniques used for deactivation of active TPs. Also, iPT is generally carried out by applying gradually increasing manual pressure to the TPs. After the initial compression, there is a brief period of local ischemia, which is followed by blood reperfusion (hyperaemia) [11–15]. The restoration of the tissue’s energetic supply by the local blood flow leads to an acceptable metabolic state for the muscle. As a result of this procedure, the TPs become less sensitive to pain, aiding in tissue repair. Also, ART releases the TPs by locating and dissolving the scar tissue and adhesions that result in pain, weakness, stiffness, numbness, and physical dysfunction [14–17].
This study indicates a need to consider the following recommendations; future studies are recommended using different modalities of conventional physical therapy, using iPT versus ART on males with piriformis syndrome, and using iPT or ART with other manual therapy techniques for females with piriformis syndrome. in a conventional physical therapy programme, it is recommended to combine hip strengthening exercises with piriformis stretching.
Limitations
The main limitation of this study was the sample size consisted of only females, which significantly reduced the external validity of the findings. The primary variables were non-normal distributed; therefore, the results are in terms of median. it is recommended to do research on the long-term effects of iPT and ART.
Conclusions
For females with piriformis syndrome, adding ART or iPT to a conventional physical therapy programme reduces pain intensity levels, and improves hip internal rotation, lower limb functional levels, and PPT. Both techniques proved to be superior in relation to the conventional treatment; however, there is no significant difference between iPT and ART in the treatment of active TPs.