Introduction
Cellulite is a descriptive term used to characterise the topographic alteration of the skin, with a high prevalence in females [1]. This alteration is still described in the literature by various terms such as gynoid lipodystrophy, nodular lipo sclerosis, oedematous fibrosclerotic panniculopathy, or oedematous adipose panniculosis [2, 3]. Cellulite is located more commonly in the outer and posterior regions of the thigh and in the buttocks region, where adipose tissue is deposited in more significant quantities in women. However, it can still be found in the hips, periumbilical abdomen, breasts, posterior region of arms, and neck [1, 4].
Cellulite is considered a multifactorial alteration initially discussed only as a visual aesthetic condition. Still, recent studies have discussed the pathogenesis of this alteration being influenced by metabolic and vascular impairments of the organism [3–5]. despite being an alteration extensively discussed in the literature and clinical practice, the understanding of the patho-physiology of the alteration still presents some questions to be answered [5]. it is believed that cellulite is the result of anatomical alterations of the subcutaneous adipose tissue associated with hormonal, vascular, and inflammatory alterations of the tissue, which culminate in the increase of the underlying subcutaneous fibrous septa and a reduction in the normal blood flow and lymphatic circulation [5–7].
The proposed cellulite treatments are diverse and widely used in clinical practice, with manual treatments being in a group that is always suggested as an auxiliary or individual treatment to improve the alteration [3, 8, 9]. Within manual treatments, manual lymphatic drainage (MLd) stands out as a technique that, when used alone or associated with other treatments such as exercises and/or physical modalities, improves the general appearance of the alteration, in addition to promoting important benefits for the bodily tissue since lymphatic and blood circulation is directly stimulated [8–10].
MLd uses specialised and distinct manoeuvres, performed with soft, slow, rhythmic, and relaxing digital pressure in the direction of the lymphatic system (vessels and lymph nodes) with different purposes. Among the goals is the drainage of accumulated fluids between spaces and interstitial cells, mainly in the dermis, to improve tissue appearance [11, 12]. it is important to point out that in recent years there has been an increase in the performance of self-drainage supervised by professionals to expand the benefits of these techniques, favouring different treatments [13, 14]. in clinical practice, MLd is often associated with the performance of physical exercises to enhance results in treating several alterations [15, 16]. Thus, it is believed that a possible association of MLd with a particular group of kinesiotherapeutic exercises may be effective in treating body aesthetic dysfunctions. Given what was presented, the objective of the present study was to evaluate the effects of self-MLd associated with supervised kinetic exercises in the treatment of cellulite and improvement in the quality of life (QoL) of patients.
Subjects and methods
Sample
Participants were recruited through digital platforms, initially including 50 participants, randomly divided into two groups: 25 participants in the control group (CG) utilising only dietary control and 25 participants in the treatment group utilising dietary management, exercises, and self-MLd (EMG).
The participants were selected according to the following inclusion criteria: female, aged between 30 and 50, weighing between 50 and 85 kg, with cellulite in the buttocks and thigh regions, multiparous or nulliparous, with or without contraceptive use, and who were sedentary. The proposed exclusion criteria included contraindications such as acute infections, malignant tumours, thrombotic disorders, severe heart failure, and severe renal failure, as well as those who did not agree to sign the informed consent form or who had inflammatory skin diseases in the treatment area, varicose veins, any therapy that could affect the treatment (chemotherapy, anticoagulant therapy, and steroids therapy) and morbid obesity (BMi > 40). Notably, the participants were instructed not to participate in any other physical activity program, treatment, or diet that could influence the study. in addition, they were also advised not to start using any type of cosmetics in the target area.
Assessment instruments
Gynoid Lipodystrophy Classification Protocol
To classify the degree of cellulite, all participants were initially evaluated by a trained professional in person one week before the start of treatment (T0) using the Gynoid Lipodys-trophy Classification Protocol (GLCP/PAFEG) [17], which is a data collection instrument that allows grading cellulite and the levels of sensory changes resulting from this condition. it should be noted that the PAFEG was reapplied one week after the end (TF) of the proposed interventions in both studied groups.
Quality of Life assessment
The CelluqolTM questionnaire was used to assess the QoL of individuals with cellulite [17]. The lower the score obtained in the questionnaire, the better the individual’s QoL concerning cellulite. in addition, the Short Form Health Survey (SF-36) translated into Portuguese was also used to assess the health-related QoL (HRQoL) of individuals. The SF-36 consists of eight QoL domains: functional capacity (FC), limitation due to physical aspects (PA), pain, general health status (EGS), vitality, social aspects (AS), emotional aspects (AE) and mental health (SM). it also has two components to summarise the physical and mental components (PCS and MCS, respectively). The items are evaluated, giving a result for each question, then later transformed into a scale from 0 to 100, where zero is considered the worst and 100 is the best [18].
The instruments were applied one week before the beginning of the interventions and one week after the end of the treatments for both groups.
Electrical bioimpedance
The GymaTM – Body Fat Analyzer (Gessate (Mi) – italy) was used. The test was performed with the individual lying on a non-conducting surface, supine, with arms and legs abducted at 45° range of motion. The volunteers were instructed to fast for 8 hours; not perform strenuous physical exercises 12 hours before the test; not drink alcohol 48 hours before the test; empty the bladder at least 30 min before the assessment, and remove metallic objects from the electrode placement site at the time of the test. The analysed variables were the percentage of total body fat (%BF) and the percentage of water in the body (%BW).
As with the questionnaires, bioimpedance was performed one week before treatment started and one week after the end of the interventions.
Anthropometric measurements
A FiberTM measuring tape was used to measure the circumference of the lower limbs at four points: the greater trochanter of the femur, on the knee over the upper edge and the lower edge of the patella, and on the ankle above the medial and lateral malleoli. The anthropometric measurements were performed on the same days as the other evaluations.
Satisfaction analysis
At the end of the treatment, after one week, the participants answered the questionnaires adapted from the patient satisfaction analysis by Segot-Chicq et al. [19] and the Global Aesthetic improvement Scale – GAiS by Narins [20], which is used to classify the response to treatments, allowing a comparative assessment at different times after the therapeutic interventions.
Intervention
Both groups underwent dietary monitoring by a trained nutritionist. The diet employed was based on caloric retention. in addition to the diet employed, the EMG performed the self-MLd protocol associated with supervised kinetic exercises by a trained professional through virtual assistance with a camera throughout the entire execution. The sessions were held twice weekly, totalling 16 sessions over two months, and each session lasted approximately 50 min.
The self-MLd protocol with exercises was based on seven moments:
Active movements to induce an increase in the contractile frequency of the lymph nodes.
Diaphragmatic breathing.
Centripetal manual pressure towards the lymph nodes.
Compression to stimulate and activate the main lymph nodes (cervical, inguinal, axillary, and popliteal).
Global stretching (upper and lower limbs, neck, and trunk).
Reduction of intra-abdominal pressure through hypopressive techniques.
Elevation of the lower limbs in favour of gravity to facilitate lymphatic flow.
Results
Four of the 50 participants who entered the study were excluded because they abandoned treatment at the beginning of the study, one from the EMG and three from the CG. Thus, the analyses presented here refer to 22 participants from the CG and 24 from the EMG. demographic characteristics are shown in Table 1. it can be seen that the mean age for both groups was similar, as well as the mean initial and final body weight.
Table 1
Demographic characteristics of the CG and EMG
| Weight (kg) | Age (years) | ||
|---|---|---|---|
| initial | final | ||
| CG | 64.21 | 64.27 | 38.2 ± 4 |
| ENG | 62.4 | 61.6 | 36.7 ± 3 |
For the cellulite grading analysis, PAFEG was used, with its initial and final classification shown in Table 2. initially, both groups had a similar distribution in terms of cellulite grade. However, at the final moment, it was observed that the EMG showed a significant reduction in the percentage of participants who had cellulite grade ii (initial: 45%, final: 25%) or iii (initial: 45%, final: 10%).
Table 2
Classification of cellulite according to the PEFAG questionnaire before and after treatment for the CG and EMG
| CG | EMG | |||
|---|---|---|---|---|
| initial | final | initial | final | |
| Grade i | 10% | 30% | 10% | 65% |
| Grade ii | 55% | 45% | 45% | 25% |
| Grade iii | 35% | 25% | 45% | 10% |
In the analysis of QoL in individuals with cellulite evaluated by CelluquolTM, it was possible to observe a significant intra-group reduction in the scores for both groups at the initial moment (CG = 32, EMG = 35) compared to the final one (CG = 12, EMG = 9). in the evaluation between groups, at the end of treatment, despite a significant difference between scores, both groups obtained the same classification according to the questionnaire (Figure 1A).
Figure 1
Quality of Life assessment using the CelluquolTM and SF36 questionnaires. A – CelluquolTM: quality of life of individuals with cellulite before (initial) and after treatments (final) in the CG and EMG, B – SF 36: assessment of overall quality of life or individuals before (initial) and after treatment (final) for the CG and EMG

For analysis with SF 36, it was also possible to observe improvement in the QoL of individuals in the intragroup evaluation when comparing the initial (CG = 44, EMG = 45) and final moments of treatment (CG = 76, EMG = 86) in both groups. At the end of treatment, there was a significant difference between the EMG (86) compared to the CG (76), demonstrating a more significant overall improvement in QoL for the EMG.
In the electrical bioimpedance analysis, total body fat percentage (%BF) and total body water (%BW) were evaluated. For the %BF, an intragroup statistical difference was observed for both groups. That is, the CG showed a reduction in the %BF at the end of the treatment (initial: 30% ± 7.1, final: 26.9% ± 8), as well as the EMG, which presented with an average of 30% ± 5.8 at the beginning, and after treatment, it showed an average of 24.4% ± 7. A difference was also observed between groups at the end of treatment, in which the EMG (24.4% ± 7) showed a significant reduction when compared to the CG (26.9% ± 8, Figure 2A).
Figure 2
Evaluation by bioelectrical impedance. A – analysis of the total body fat variable before and after treatment for the CG and EMG, B – analysis of the variable amount of total body water before and after treatment for the CG and EMG

For the %BW analysis, intragroup differences were observed for EMG and between groups at the end of treatment, with a significant reduction being observed between the initial (34.8% ± 3) and final (29.9% ± 2.2) assessments for the EMG and a statistical difference between the CG (32.6% ± 3.1) and EMG (29.9% ± 2.2) at the end of treatment (Figure 2B). For analysis of the left ankle’s anthropometric measurements, it was impossible to observe significant intragroup and intergroup differences (Figure 3A). However, in the anthropometric measurements of the right ankle, it was possible to observe a significant reduction in the initial (23.3 ± 1.7) and final (20.1 cm ± 1.6) assessments for the EMG. Furthermore, when comparing groups at the end of treatment, significantly smaller anthropometric measurements were observed for the EMG (20.1 cm ± 1.6) compared to the CG (24.1 cm ± 2.3). in the intragroup analysis for the anthropometric measurements of the right knee (upper edge) in the EMG, a significant reduction was observed at the beginning (44.4 cm ± 2.6) compared to the end (41.3 cm ± 2.6) of treatments. Furthermore, a significant difference was found at the end of treatment in the EMG (41.3 cm ± 2.6) compared to the CG (45.8 cm ± 3.6, Figure 4A).
Figure 3
Ankle circumference. A – measurement of the left ankle circumference before (initial) and after (final) treatment for the CG and EMG, B – measurement of the circumference of the right ankle before (initial) and after (final) treatments for the CG and EMG

Figure 4
Knee anthropometric measurements. A – measurement of the circumference of the right knee (upper edge) before (initial) and after (final) treatment for the CG and EMG, B – measurement of the circumference of the left knee (upper edge) before (initial) and after (final) treatments for the CG and EMG

Notably, no significant differences were observed for the anthropometric measurements of the left knee (upper edge) in the intragroup and intergroup analyses (Figure 4B).
For the perimeters of the left knee (lower edge) and the right knee (lower edge), a significant reduction was observed in the intragroup analysis when comparing the initial (right: 35.7 cm ± 2.1, left: 35.8 cm ± 2) and final (right: 32.1 cm ± 1.8, left: 31.9 cm ± 1.8) in the EMG (Figure 5). For both sides of the knee (lower border), a statistical difference was also observed at the end of treatment in the EMG (right: 32.1 cm ± 1.8, left: 31.9 cm ± 1.8) compared to the CG (right: 36.2 cm ± 2.7, left: 36.1 cm ± 2.6, Figure 5). in the anthropometric measurements on the greater tro-chanter, the intragroup analysis for both sides showed that the EMG presented a significant reduction in the initial circumference (right: 59.6 cm ± 3, left: 59.9.8 cm ± 3.7) when compared to the final measurements (right: 54.9 cm ± 2.1, left: 54.5.8 cm ± 3.1). in addition, the analyses between the groups showed a statistical difference on both sides between the EMG (right: 54.9 cm ± 2.1, left: 54.5.8 cm ± 3.1) when compared to the CG (right: 60.7 cm ± 5, left: 60.5 cm ± 5.4) at the end of treatment (Figure 6).
Figure 5
Knee anthropometric measurements: A – measurement of the circumference of the right knee (lower edge) before (initial) and after (final) treatment for the CG and EMG, B – measurement of the circumference of the left knee (lower edge) before (initial) and after (final) treatments for the CG and EMG CG – control group, EMG – group with a combination of diet, exercise, and self-lymphatic drainage * statistical difference in intragroup comparison (initial vs final) (p 0.05), # difference in the comparison between groups (CG vs EMG) (p 0.05)

Figure 6
Anthropometric measurements over the greater trochanter of the femur: A – measurement of the circumference over the greater trochanter of the left femur before (initial) and after (final) treatment for the CG and EMG, B – measurement of the circumference of the greater trochanter of the right femur before (initial) and after (final) treatments for the CG and EMG

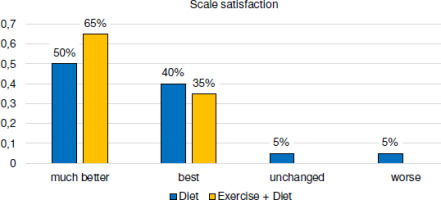
The assessments regarding patient satisfaction after treatment are shown in Figure 7. it is possible to observe that the EMG group had a more satisfactory response in this regard than the CG since 65% of the EMG participants reported “much better” satisfaction compared to 50% who got the same response as the CG. it is also possible to observe that 10% of the participants in the CG group did not show significant satisfaction with the treatment, with “worse” and “unchanged” responses being presented for this group.
Discussion
In recent years, studies addressing cellulite treatment have grown exponentially, mainly because this alteration is discussed not only as an aesthetic condition but as an alteration that causes significant damage to the body at the circulatory level [3, 5]. Within this context, in clinical practice and the literature, MLd is widely discussed as a highly effective manual treatment for various body aesthetic dysfunctions [10, 12, 21]. However, scientific studies regarding the application of MLd in cellulite are still scarce, especially those who approach the technique in a self-administered way. it is important to emphasise that the clinical studies that evaluate cellulite treatments, for the most part, are not randomised or controlled. in addition, the evaluations are subjective, based on the patient’s opinion and the comparison of photographs, which are not always done in a standardised way [22]. Thus, the debate between studies is hampered.
The present study sought to discuss the effects of the association of a physical exercise protocol and self-MLd in the treatment of cellulite in women who simultaneously underwent a calorie-restricted diet, with significant reductions in %BF and %BW being observed, in addition to the reduction the diameter of different areas. it is also noteworthy that the treatments employed improved the QoL of individuals and significantly improved the degree of cellulite.
Recent studies have shown that the effectiveness of treatment with MLd in cellulite is more successful when associated with a group of exercises, diets, or physical modalities that have adipose cells as the target of application [9, 12, 23, 24]. These associations are effective since they are based on the pathophysiology of the alteration [4, 8], in which the increase in adipose cells influences the development of cellulite. our study corroborates these discussions since the association of diet with self-MFd and exercises improved the degree of cellulite and body contour, supported by anthropometric measurements and bioimpedance analyses.
Smalls et al. [23] presented a study that evaluated the improvement of cellulite after the prescription of a restricted caloric diet, having observed positive results with most participants regarding the reduction in the %BF and improvement of the general tissue appearance. However, in some cases, the authors highlighted that diet and weight loss were insufficient to improve a significant part of the cellulite picture. This data corroborates our study since both groups, who underwent a calorie-restricted diet, showed a significant improvement in the appearance of the skin and a reduction in the %BF. However, it was also observed that in the group that, in addition to the diet, performed the self MLd and exercises, the data regarding the decrease in the degree of cellulite, %BF, %BW, and anthropometric measurements brought more relevant results than the group that only performed diet. it is noteworthy that the same study by Smalls et al. [23], highlighted that despite the reduction in the %BF after the diet, the patient’s body weight showed no difference, as well as in our study, in which the initial and final weight for both groups were very similar.
Rostom et al. [9] carried out a randomised study that evaluated 30 women with cellulite, after two months of treatment with two different MLd approaches. The study assessed the involution of cellulite using the Cellulite Severity Scale, having obtained a significant improvement in the condition regardless of the MLd method applied. As in our study, it was observed that the application of auto MLd associated with diet presented superior results regarding the involution of the degree according to the evaluation instrument used PAFEG, demonstrating that the association of treatments potentiates the effects already discussed in the literature.
Performing self-massage is already discussed in several areas as an auxiliary treatment resource for various disorders [25–27]. in recent years, with technological advances and different realities, the search for additional resources that can be performed by the patient, with professional supervision, has increased. The CoVid-19 pandemic expanded this reality even more to encourage self-care and maintain some treatments that could be supervised through online applications called teleassistance [27–29]. Within this context, the present study reaffirms that the addition of telehealth and self-massage are effective for some dysfunctions, such as treating cellulite.
Godoy and Godoy [30], discussed that any type of external compression towards the lymphatic flow that promotes a pressure differential between the extremities could displace the fluid contained in a conduit and thus promote benefits to the system, reporting that the patient can perform these movements, corroborating the present study in which the volunteers themselves conducted standardised manoeuvres towards the lymphatic system, thus obtaining promising results in the treatment of cellulite.
The forms of evaluation of cellulite treatment are still extensively discussed in the literature, mainly because it is an alteration that affects the entire integumentary structure of the affected area [5]. Classification by scales, in addition to anthropometric measurements, are resources widely used in the literature. de Almeida et al. [24] treated ten women with grade i and iii cellulite using MLd and ultrasound and observed, through thigh and knee anthropometric measurements and evaluation using scales, an important reduction in the degree of cellulite, especially those classified as grade iii, in addition to a decrease in anthropometric measurements achieved after treatment. in our study, it was observed that the group that presented greater involution of the degree of cellulite also showed a significant reduction in the evaluated diameters, in addition to a more substantial response in the questionnaires.
The discussion about psychosocial impairment caused by cellulite is a topic that is currently widely discussed. Meyer et al. [31] report several problems caused by the demand for aesthetic standards of the present day, highlighting that the analysis of QoL and patient satisfaction are extremely relevant measurements in studies that address this theme. The present study sought, in addition to analysing the physiological improvement of cellulite, to also evaluate the psychosocial impact of the treatments on the participants. Thus, it is possible to report that the participants who received self-MLd with exercises associated with a diet showed a significant improvement in QoL and greater satisfaction after treatment. despite the present study being a randomised clinical trial with an important sample size, some limitations and future suggestions can be made from the study presented here. it is believed that because it is a method that the patient can perform, a larger number of participants would be recommended to confirm the effects presented here, always remembering that a trained professional must supervise the technique.
Conclusions
Through the data presented, it is possible to conclude that a diet with caloric restriction presents a significant improvement in individuals with cellulite. However, when associated with self-MLd, these results are potentiated both for the corporal improvement, obtained through the results of the bio-impedance and anthropometric measurements, as well as the psychosocial improvement, shown by the QoL and personal satisfaction questionnaires.