Introduction
Shoulder impingement syndrome (SiS) is consistently recognized as one of the most commonly diagnosed shoulder conditions [1]. in the literature, it is noted that shoulder impingement is believed to be a factor in nearly 48–65% of all cases involving a painful shoulder condition [2]. it does not refer to a specific pathological condition in the shoulder; instead, it encompasses a range of disorders, typically associated with pain, characterized by inflammatory and degenerative modifications of the soft tissues near the subacromial region [3].
The scapulohumeral rhythm (SHR), which refers to the coordinated coupling of motion between the scapula and humerus, is essential for effective arm motion [4, 5]. during abduction, decreased mobility of the scapula causes a reduction in the acromiohumeral distance which increases the possibility of generating SiS [6]. Evidence proposes that patients suffering from rotator cuff diseases and various shoulder impingement symptoms exhibit an alteration in scapular kinematics otherwise known as “scapular dyskinesis” [7].
The force output and muscle imbalance of scapulothoracic muscles, as well as balanced recruitment time among these muscles, might be correlated to shoulder impingement and could have implications for conservative treatment [8].
Symptoms of subacromial impingement include pain, disability, and increased scapular anterior tilt with decreased scapular upward rotation [9]. Changes in scapular positioning and muscle imbalance of the scapulothoracic muscles are considered important risk factors for developing SiS.
According to previous research studies [10–13], the majority of exercise programs highlight the significance of scapular training as a fundamental element in shoulder rehabilitation which aims at restoring proper scapular posture and movement patterns [5, 14].
Clinical prediction rules (CPRs) are asserted to aid clinicians in making informed clinical decisions concerning diagnoses, prognoses, and the selection of interventions tailored to individual patients. These methods rely on certain predictor variables derived from the initial assessment of the patients during history taking and physical examinations [15–18].
To the authors’ knowledge, there is a lack of adequate research that identifies certain examination variables that might be of predictive value for which patients will successfully respond to scapular muscle training. Hence, the identification of the aforementioned variables would be of added value to the clinical decision-making process and may aid in improving the effectiveness of proposed interventions and treatment plans. Thus, the development of a clinical prediction rule (CPR) to select participants who would benefit from scapular musculature training exercises would improve the clinical decision-making process, minimize the duration of treatment, and optimize clinical outcomes.
Therefore, this study aimed to determine whether the scapular upward rotation angle, pain severity, functional disability, and upper trapezius/serratus anterior (UT/SA) isometric strength ratio at the baseline assessment can predict the response of patients to scapular training in cases of subacromial impingement syndrome (SAiS). We hypothesize that these variables will serve as effective predictors of scapular muscle training outcomes in patients with SAiS.
Subjects and methods
Design
A clinical predictive study was conducted on patients with SAiS for four weeks in the outpatient physiotherapy clinics of Cairo University. The time taken to recruit the subjects was from September 2020 to April 2021.
Participants
An orthopedic surgeon screened patients who had been diagnosed with SAiS, according to Neer’s classification specifically in stages i and ii. Neer outlined three stages of impingement syndrome. in stage i, the patient has reversible edema and hemorrhage. The supraspinatus tendon was inflamed, which is the reason for the aching discomfort experienced by these patients. Stage ii entails fibrotic alterations in the supraspinatus tendon and subacromial bursa that produce pain with movement and are typically observed in patients between the ages of 25 and 40. Stage iii occurs in adults over 40 who have a history of shoulder pain, and either a partial or full-thickness tear in the rotator cuff [19].
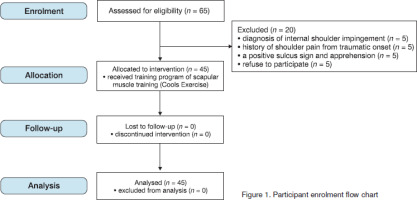
A total of 65 male and female patients from the outpatient clinic at Cairo University were assessed for eligibility. To facilitate blinding, measurements were taken to ensure that outcome assessors and data analysts were kept uninformed of the specific hypotheses under examination and the clinical characteristics of participants relevant to the prediction rule. An independent researcher, uninvolved in any other aspect of the study, operated to allocate patients to the interventions. This person was solely responsible for this task to ensure the exercise supervisor remained unaware of the participants’ baseline measurements as pre- and post-measurements. Fifteen patients were excluded from the study for not meeting the inclusion criteria, and an additional five patients declined to participate, as depicted in Figure 1, in accordance with the SiAS inclusion and exclusion criteria detailed in Table 1.
Table 1
Inclusion and exclusion criteria of the present study inclusion criteria individuals diagnosed with SAiS and aged between
Sample size
G*PoWER© software (ver.3.1.9.2, Heinrich-Heine-University, düsseldorf, Germany) with priori testing was used to calculate the adequate sample size, using a significance level of 5%, a power level of 90%, and a medium effect size (Cohen’s d = 0.25). The mean difference used in this study was 5 degrees of scapular upward rotation angle based on a similar study [20]. Based on these assumptions, it was estimated that the sample size needed for this study was a minimum of 45. Following the literature research 10–15 patients were required for each predictor variable in the study, and five individuals were set aside as dropout candidates [15, 21].
Outcome measures
Shoulder pain and functional disability
The Shoulder Pain and disability index (SPAdi) is a self-administered questionnaire designed to assess both disability and pain associated with shoulder conditions in individuals experiencing shoulder pain, whether it is due to musculoskeletal, neurogenic, or unknown causes [22]. The SPAdi contains 13 items that evaluate two domains: the first domain is a 5-item pain scale and the second one is an 8-item disability scale [23].
The SPAdi usually takes around 5 to 10 min to complete with the literature investigating the Arabic version of the SPAdi showing a higher inter-rater agreement, validity, and methodological qualities. it also showed high test-retest reliability and construct validity [24, 25].
Scapular upward rotation angle
Two bubble inclinometers were utilized to measure the upward rotation of the scapula. These inclinometers have a 360-degree rotating dial with a fluid indicator (Baseline® Bubble inclinometer, Fabrication Enterprises iNC, White Plains, New York 10602, USA). The literature shows that the bubble inclinometer is considered a valid and reliable way to assess the upward rotation of the scapula in all ranges of shoulder abduction in the coronal plan. These inclinometers were positioned above humeral epicondyles and on the scapula’s superior surface. With good interrater reliability (iCC score of 0.88), they effectively assessed scapular upward rotation in various abduction ranges. Patients, standing barefoot, performed 100° of shoulder abduction with the inclinometers recording readings. The methodology, validated in prior literature, proved efficient, providing a standardized approach for measuring scapular upward rotation in the coronal plane during specific shoulder movements [26, 27].
Measuring of muscle strength ratio
Assessed using the handheld dynamometer (HHd). it provides a more objective evaluation approach that is significantly superior to manual muscle testing when measuring changes in muscular strength. The Hdd provides acceptable validity and reliability in the assessment of shoulder and scapular muscles [28, 29].
The model used was a Nicholas manual muscle tester (Model 01160, Lafayette instrument Co., Lafayette, iN). For the upper trapezius, the patient was seated with the dynamometer being placed on the superior scapula and the patient was asked to shrug his shoulders up. As for the serra-tus anterior, the patient was placed supine with the shoulder and elbow at 90° flexion, and the resistance was applied along the axis of the humeral head passing through the ulna, then the UT/SA isometric strength ratio was calculated [30].
Intervention procedure
The interventions were performed three times per week for four weeks with 10 repetitions per set for a total of three sets and having a rest time of 1 min between each set, with a 10-repetition maximum (RM) testing being used to determine the resistance to be applied. The maximum weight where the load could be done for ten repetitions was used. Scapular muscle training (Cools exercises) often focuses on improving scapular muscle imbalance and is considered ideal for restoring the balance among the upper, middle, and lower fibers of the trapezius muscle [7, 14, 31, 32]. The exercises performed as shown in Figure 2. in addition, serratus anterior strength training was performed by laying supine on a bench, keeping the shoulder at 90° flexion with the elbow completely extended, protracting the scapula to its end range [33].
Figure 2
Scapular muscle training (Cools exercises) for restoring the balance among the upper, middle, and lower fibers of the trapezius muscle. The image shows the sequence of training: A – forward flexion in a side-lying position, B – side-lying external rotation, C – horizontal abduction with external rotation, and d – prone extension
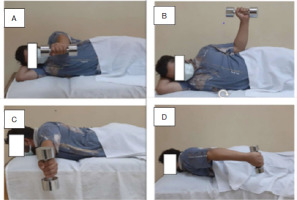
A. Forward flexion in side-lying: in this exercise, the patient is guided to lie on their side with the shoulder in a neutral position. They are then directed to flex the shoulder to 135° while maintaining the side-lying posture.
B. Side-lying external rotation: in this exercise, the patient is advised to lie on their side with the shoulder in a neutral position and the elbow flexed at 90°. A folded towel is placed between the patient’s limb and trunk to prevent compensatory movements. The patient is then guided to externally rotate the shoulder while keeping the elbow at 90° of flexion and ensuring the towel remains in position.
C. Horizontal abduction with external rotation: For this exercise, the patient is directed to lie prone with their arms hanging outside the bed, and the shoulders should be relaxed with 90° of shoulder flexion. Subsequently, the patient is guided to execute horizontal abduction, bringing the arms to the horizontal position, and incorporating external rotation once maximum abduction is achieved. d. Prone extension: in this exercise, the patient is guided to lie prone with their arms extended outside the bed, and their shoulders should be relaxed with 90° of flexion. The patient is then instructed to extend the shoulders back to a neutral position while keeping the shoulder rotation in a neutral position as well.
Statistical analysis
The statistical package for social studies (SPSS) version 26 for Windows was used to provide all statistical analysis (SPSS inc., Chicago, iL, USA). Based on a minimal clinically important difference (MCid) for each dependent variable, participants were grouped according to the result (success or failure).
The MCid was defined as the smallest difference in score in the domain of interest which patients perceive as beneficial and which would necessitate a change in the management of the patient, provided there are no significant side effects or excessive costs [34], according to the definition provided by Jaeschke et al. [35] Patients who matched the reference criteria was considered to have successful treatment.
The study evaluated statistically significant continuous independent variables using RoC curves, representing the balance between sensitivity and specificity. optimal cutoff points for distinguishing success and failure were determined by plotting sensitivity against 1 minus specificity in the analysis.
Results
Forty–five patients with SAiS participated in this study with their demographic characteristics at baseline as well as the distribution of the variables within the intervention group shown in Table 2.
Table 2
Baseline characteristics of all participants (n = 45)
Calculating the mean difference for pain, scapular upward rotation angle disability, and the strength ratio of the upper trapezius to serratus anterior muscle to determine patient response. A reference criterion to determine which patient had a successful or unsuccessful outcome was predetermined. This criterion was (1) a decrease in SPAdi value for pain by 20% or more, and (2) an improvement in SPAdi value of functional disability at least by 20%, this is the MCid for SPAdi [23].
Test-retest reliability of the upward rotation of the scapula angle has been reported to range from an iCC = 0.88 and a MCid from 0.81 (at 100°) to 0.94 (at both resting and end of total shoulder abduction range) [26]. The MCid for scapular muscle strength was a UT/SA ratio score that increased by 0.2 points [27]. The success rate was 88%, where 40 patients were considered to have a favourable response to scapular training according to the reference criterion that was predetermined. These results are shown in Table 3.
Table 3
The success rate of different studied outcomes
The results revealed a significant difference between preand post-scapular training tests with regards to pain in percentages (25 ± 14.5, 63 ± 20, respectively), disability in percentages (17 ± 10, 52 ± 20, respectively), upward rotation angle (26 ± 6; 30 ± 5, respectively), and UT/SA strength ratio (1 ± 2, 1.5 ± 0.7, respectively), and a p-value < 0.05 as shown in Table 4.
Table 4
Distribution of outcome measures and the correlation between results of the patients before and after using the scapular training
Analysis of variance
To determine at which point the variables were most predictive to benefit successfully from scapular muscle training, as well as to determine the specificity and sensitivity values a receiver operating characteristic curve (otherwise known as RoC curve) was used. The results showed that in patients with SAiS, the pain and disability percentage as well as the UT/SA strength ratio all obtained at baseline assessment had high sensitivity in terms of predictor value for the patient’s response to scapular training.
The results for pain percentage showed promise with the area under the curve (otherwise known as AUC) being equal to 0.93, with a sensitivity of 0.9 and a specificity of 0.33, it could be a predictor if 31.32. As for the results of the disability percentage, they also showed promise with the AUC having a score of 0.94, with a sensitivity of 0.956 and a specificity of 0.156, it could be a predictor if 30.85. The UT/SA strength ratio showed promising results as well, having an AUC of 0.9, with a sensitivity equaling 0.9 and a specificity equaling 0.33, it could be a predictor if 1. Unlike the aforementioned variables, the upward rotation angle showed poor results with an AUC of 0.66, a sensitivity of 0.62, and a specificity of 0.36, it could be a poor predictor if 28.5 as shown in Figure 3 and Table 5.
Figure 3
Descriptive statistics and RoC curve, demonstrating area under the curve (AUC), sensitivity and specificity of interfering with this procedure, and cut-off points for pain, disability, scapular upward rotation angle, and upper trapezius/serratus anterior strength ratio (UT/SA)
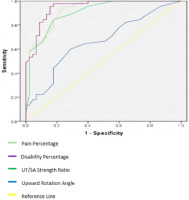
Table 5
Description of sensitivity, specificity, and cut-off points represented by the RoC curve
Discussion
SAiS is a common musculoskeletal condition, that involves compression of the tendons and bursa within the shoulder joint, leading to pain and restricted movement. Several studies have explored various treatment modalities for musculoskeletal pain, aiming to alleviate symptoms and improve function [36, 37]. For practicing clinicians, the capability to expect which patients would respond better to a certain treatment intervention may be extremely useful. Therefore, the study aimed to figure out which variable is predictive at the baseline assessment (pain, disability, UT/SA isometric strength ratio, and the angle of scapular upward rotation) associated with the successful implementation of scapular training and its positive outcomes for individuals diagnosed with SAiS.
The results of our study showed that pain severity, functional disability, and the UT/SA ratio were of excellent predictive value, whereas the upward rotation angle of the scapula was of poor predictive value. in addition, the findings of this study pointed out that Cools exercises are an effective intervention for reducing pain, enhancing functionality, increasing scapular upward rotation, and bolstering scapular muscle strength in individuals dealing with SAiS with a success rate of up to 88%.
With regards to pain, there is evidence that suggests this syndrome is one of the most common complaints in patients with SAiS and is characterized by being chronic and/or relapsing that could be due to the compressive forces of the humeral head to the subacromial bursa, rotator cuff, or both structures causing persistent inflammation of the soft tissues [8]. These results align with the outcomes of various other studies that also concluded that scapular training was not only beneficial in pain management but also in enhancing scapular movement and reducing overall disability in individuals who were diagnosed with SAiS, as reported by Reijneveld et al. [38]. in addition to that, a study by Gebremariam et al. [9] included interventions that focused on rotator cuff strengthening for SiS treatment, with an emphasis on the infraspinatus and supraspinatus, as well as serratus anterior and trapezius strengthening resulted in large improvements in pain scores.
Concerning the description of the RoC curve analysis, the findings revealed that pain levels at the initial assessment serve as a predictive factor for the efficacy of scapular training in patients diagnosed with SAiS. Patients are more likely to benefit from scapular training if their baseline pain value is either bigger than or equal to 31.32. other studies support our results and found that adding scapular stabilization exercises was more beneficial in improving scapular muscle strength, preventing scapular dyskinesis, decreasing pain, and improving function [10, 39].
Additionally, the results demonstrated that disability at the baseline assessment is also an indicator of the efficacy of the training of the scapula in individuals with SAiS, with patients showing the best response when their baseline disability score is greater than or equal to 30.85. The time length of shoulder pain and main functions are significant predictive factors for physical therapy treatment for shoulder pain, according to prior evidence [40].
These findings are compatible with the research conducted by Kristensen et al. [41], who investigated the impact of scapular–focused exercises with scapular stabilization on patients with SAiS. Their study also reported improved patient-rated outcomes, including reduced pain levels and enhanced function, range of motion, and strength [41]. Additionally, another study exploring the effects of a scapular training program on impingement syndrome found that exercises targeting the scapula effectively alleviated impingement symptoms. This included improvements in pain and disability of the shoulder, in addition to enhancements of the kinematics in the shoulder joint, such as upward rotation, anterior tilt, and internal rotation [42].
The results also suggest that the UT/SA strength ratio at the baseline assessment serves as a predictor for the efficacy of scapular training in patients who suffer from SAiS, with the best response observed when its value is larger than or equal to one. A previous study by de Mey et al. [32] indicated that scapular muscle rehabilitation exercises in patients with impingement symptoms resulted in decreased amounts of trapezius muscle activation which in turn caused the UT/SA ratio to be remarkably reduced, whereas UT/MT and UT/LT were constant. Rather than being a direct outcome of the training program, such changes in muscle activation levels after training might be produced by neural adaptations linked with short–term exercise training. it was suspected that the reason behind the UT/SA strength ratio having had positive potential for being a predictor had to do with the static and dynamic properties of the scapula and their role in SAiS. The co-contraction of the UT/SA produces controlled motion of the scapular upward rotation when the shoulder is in elevation; this, in turn, maintains a healthy scapulothoracic rhythm and adequate subacromial space. inversely, an overactivity of the upper trapezius and reduced serratus anterior activity (so an increased ratio) is seen in many athletes with subacromial impingement leading to the rationale that maintaining healthy dynamic movement of the scapula through a balanced UT/SA ratio is important in the prevention of SAiS and hence would serve as a positive predictor for the success rate of training of scapular muscle in the treatment of SAiS [43, 44].
However, the findings indicate that the upward rotation angle at the baseline assessment has limited sensitivity in predicting the condition; this diminishes its reliability as a predictor for the success of scapular training in individuals who were diagnosed with SAiS, even when its value is 28.5 or higher. This may be explained by the fact that the static positioning of the scapula measured at a stop of shoulder elevation would not be the primary cause of SAiS, rather the dynamic movers behind it and thus the scapular upward rotation measured in a static pause of shoulder elevation proved to be a poor predictor in this study. Not only that, but the evidence suggests that although patients with SAiS experience decreased scapular upward rotation, the actual subacromial proximity areas and prevalence of contact between the rotator cuff and the subacromial arc were not prevalent in these individuals when compared to individuals with higher upward rotation angles [45]. Hence, the upward rotation angle of the scapula, though reduced in patients with SAiS, would not significantly affect the rotator cuff tendons or cause more symptoms. This could explain the poor predictive results observed in this study. our findings underscore the importance of carefully considering the appropriateness of Cools exercises in certain contexts. While our study provides valuable insights into the potential limitations of these exercises, it’s crucial to note that our results primarily suggest when not to use them, rather than when to use them. This nuanced understanding is vital for clinicians and researchers alike, as it highlights the need for tailored exercise prescriptions based on individual needs and circumstances.
Limitations
One significant limitation that remains unaddressed pertains to the observed high sensitivity and low specificity across all tests utilized. This characteristic poses a considerable risk of yielding false positive results and represents cases where these tests may offer meaningful insights. However, their efficacy diminishes when attempting to accurately identify positive cases, thereby highlighting a notable constraint in their applicability. Additionally, it’s important to recognize that improvement after scapular muscle exercises may be influenced by numerous factors beyond those considered in this study. Another notable limitation is the duration of the training program, which was only four weeks. To fully understand the sustainability and long-term effects of the scapular training program, a longer follow-up period or extended training duration may be necessary.
Conclusions
The study suggests that pain severity, functional disability, and the UT/SA isometric strength ratio might potentially predict the efficacy of scapular training exercises for patients who suffer from SAiS. These factors showed promising results in assessing the response to scapular training. However, the scapular upward rotation angle demonstrated poorer predictive value. This indicates that these clinical variables could be considered when tailoring scapular training programs for individuals with SAiS.