Introduction
Carpal Tunnel Syndrome (CTS) is a prevalent medical disorder that affects the hand and arm of the affected person, causing discomfort, numbness, and tingling. Exerting pressure or constricting the median nerve as it traverses the wrist might lead to CTS. Obesity, rheumatoid inflammation, hereditary inheritance, pregnancy, and repetitive wrist activities are risk factors for CTS [1]. Ten times more women than men are influenced by CTS, which ordinarily shows in those between the ages of 40 and 60. The symptoms of carpal tunnel syndrome can affect both hands, orpredominantly the dominant hand. Among these are paresthaesia, stinging, pain perception, and reduced muscle strength, particularly on the side involving the three main fingers [2]. Because monotonous wrist movement puts weight on the median nerve, carpal tunnel syndrome may become more likely in individuals with limb lymphoedema, which makes treating this condition more troublesome [3]. Endoneurial oedema develops in response to problems with blood flow to the endoneurial capillary structure, caused by, i.e., mechanical injury, hypertension, or damage to the median nerve from ischemia. Within the carpal tunnel, the common pressure ranges from 2 to 10 mmHg, but when the wrist is extended or flexed, the pressure rises eight to ten times higher than this [1]. Monotonous compression of a nerve can cause demyelination at the compression location [1]. Carpal tunnel syndrome may be connected to lym- phoedema and its volume. The condition’s seriousness and conceivable treatments incorporate surgery, steroid infusions, and splinting [4]. People encountering lymphoedema report arm pain, numbness, or heaviness. Radiotherapy or nerve damage following axillary node dissection are the causes of sensory abnormalities within the affected arm, such as diminished sensation within the medial aspect of the arm [5]. Nonsteroidal anti-inflammatory drugs (NSAiDs), pharmaceutical infusions, splinting immobilisation, restoration modalities (for example, therapeutic ultrasound, stretching, as well as strengthening), and carpal tunnel release surgery are a few of the treatment alternatives available for CTS [6]. One innovative and noninvasive therapeutic approach is extracorporeal shock wave therapy (ECSWT). it is predicated on the production of acoustic waves that interact with cells directly through mech- anotransduction, causing the metabolic rate to increase and resulting in tissue remodelling [7]. There are two types of ESWT: radial ESWT (rESWT) and focused ESWT (fESWT). fESWT creates the greatest energy at a focal point located deeper within the body tissues than rESWT, which has a more superficial effect and reaches the maximum energy at the skin surface, which spreads radially into the tissue [8]. it has been shown to have proliferative, analgesic, and anti-inflammatory properties [9]. it has also been shown to have effects on peripheral nerve reinnervation [10]. Extracorporeal shock wave therapy (ESWT) has been demonstrated in multiple trials to have a lasting beneficial impact on pain reduction in conditions involving soft tissues, such as plantar fasciitis, Achilles tendinopathy, as well as tendinopathy of the shoulder and elbow [11, 12]. It shows that ESWT has two restorative effects: it diminishes delicate tissue irritation and actuates anaesthesia in nerve filaments through biomechanical changes. It is hypothesised that these variables most likely reduce CTS sufferers’ clinical side effects [13]. Previous studies [14] have centred on the efficacy of ESWT for treating persistent musculoskeletal disorders or pillar pain following carpal tunnel release.
The evidence supporting the efficacy of ESWT in treating carpal tunnel syndrome among patients suffering from postmastectomy lymphoedema remains limited, necessitating further research to elucidate its therapeutic potential. This study was conducted to examine the effects of ESWT on pain, hand symptoms and functions, limb volume, and nerve conduction velocities among patients experiencing CTS secondary to post-mastectomy lymphoedema.
Subjects and methods
Study type
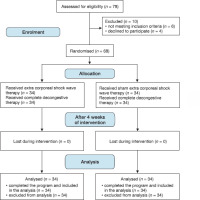
The investigation was a randomised controlled trial conducted in parallel groups, with both the patients and the assessor being unaware of the treatment assignments (double- blinded). The sample (78 subjects) were randomly selected from the outpatient clinic at the Faculty of Physical Therapy, Cairo University, Egypt. The participants were diagnosed by a physician, then referred to the clinic of physiotherapy. Ten subjects were excluded because they declined to participate in the study (4 subjects) or did not meet the inclusion criteria (6 subjects). We utilised retention methods to reduce dropout among the participants, which included reminders, phone calls, birthday cards, and reimbursement for time and expenses incurred due to their participation. In total, 68 subjects signed the consent form that was accepted by the College of Physiotherapy and were randomly allocated to two equal groups. The experimental group (n = 34), underwent focal extracorporeal shock wave treatment (fESWT) 1 session per week plus conventional physiotherapy (manual lymph drainage, compression bandage and skin care) 2 sessions per week, while the control group (n = 34) underwent sham SWT 1 session per week with conventional physiotherapy 2 sessions per week (Figure 1).
To determine if they were eligible to participate, orthopaedists and general practitioners evaluated all patients who received physical therapy for carpal tunnel syndrome (hand discomfort, paraesthesia, as well as severe swelling).
Sample-size framework
Sample size calculation was performed using the G*POWER statistical software (version 3.1.9.2; Franz Faul, Universität Kiel, Germany) expecting a large difference between group, which revealed that the primary outcome effect size was 0.7 (based on Visual Analogue Scale (VAS) data from a previous pilot study conducted on 5 subjects in each group) with a = 0.05, power 80%, n = 68, and a two-sided 5% significance level. For this study, the most appropriate total sample size was found to be 68 subjects: 34 subjects in each group.
Subjects
Inclusion criteria
Patients were enrolled in the trial if they met the specified criteria: being aged between 40 and 60 years old and presenting with mild-to-moderate CTS; experiencing hand discomfort, paraesthesia and severe oedema that worsens at night or with repetitive use of the wrist; having undergone a modified radical mastectomy and exhibiting a positive Ti- nel’s sign [15]; patients with a history of breast cancer for which they had undergone unilateral excision of the axillary lymph nodes; and presenting with mild-to-moderate, or stage i-ii lymphoedema (a difference in circumference of up to 2 cm compared to the other arm indicates a mild degree of lym- phoedema, while a difference of 2-5 cm indicates moderate lymphoedema). Patient started oncological treatment 1 month after their operation and completed it for 1 year. They participated in the study for 6 months after developing lymphoedema and for the 3 to 6 months of oncological treatment.
Table 1 displays the participants’ characteristics for both the experimental and control groups. No subject characteristics showed significant differences between the groups (p > 0.05).
Table 1
Comparison of subject characteristics among experimental group and control group
Exclusion criteria
Patients were ineligible if they had any of the following: received a steroid injection for CTS, wrist deformity that restricted the use of splints, malignant tumour mass, tendency for blood clot formation, cervical radiculopathy, brachial plexopathy, polyneuropathy or other nerve entrapment conditions in the upper extremities, previous wrist fractures, or having undergone cervical spinal or wrist surgery [16].
Program of intervention
Subjects in the experimental and control groups received conventional physiotherapy (two times per week for four weeks) in the form of 60-minute Manual Lymph Drainage (MLD) sessions, bandaging with compression, exercises, and skin care for the afflicted areas [17]. Manual lymphatic drainage (MLD) involves applying gentle pressure and gradual, rhythmic movements to facilitate the passage of lymph fluid from the affected areas towards the central part of the body. MLD begins and ends with deep diaphragmatic breathing [18]. Bandaging for Compression (CB) in the form of a multilayer, short- stretch bandage that efficiently reduces the limb volume in the acute, intensive phase of complete physical therapy (CPT) when placed on the lymph oedematous extremity after MLD [19]. Lymphoedema exercises consist of mild stretching, range-of-motion exercises, and lymphatic system strengthening. The following are some exercises for upper limb lym- phoedema: pectoral and trapezius muscle stretching; mobilisation of the shoulder girdle, which includes scapular retraction, protraction, depression, shoulder extension, elbow flexion and extension, wrist flexion and extension, as well as ball squeeze. The warm-up activity consists of actively mobilising the major joints at a moderate speed for a duration of five minutes. Diaphragmatic breathing is a technique where patients are in a relaxed state, comfortably positioned, and have their hands placed over their abdominal muscles. The technique involves inhaling deeply through the nostrils and exhaling slowly and effortlessly through the mouth [20]. Skin care is necessary to keep skin integrity intact and to lower the risk of cellulitis. The patients were instructed to keep their skin supple and silky, it is recommended to prevent dry and cracked skin by taking care of the skin daily, which includes cleansing, moisturising, and inspection [21]. Over the whole duration of the trial, no patients reported any instances of infection or adverse consequences related to the increased volume of their limbs. Prior to each session, a comprehensive evaluation of the patients was conducted. if any wounds or injuries were present, the sessions were rescheduled until the healing process was fully completed. Each female participant in the trial received guidance on how to properly care for the skin of the affected limb based on their specific clinical condition and requirements. They were instructed to keep the limb elevated whenever feasible.
ECSWT for experimental group
Participants in the study group were given focal ECSWT from Physio Shock Wave Therapy system (Pagani Elettronica, Milano, italy) one session per week, over four successive weeks. At the start of each session, patients would sit comfortably with their forearm and fingers resting on the table as ESWT was delivered to them. With the palm facing upwards, the median nerve was located in the pisiform area of the proximal carpal tunnel. Along the median nerve, the treated area went from the level of the pisiform bone to a point 2 cm before the opening of the carpal tunnel. The ESWT probe was positioned perpendicular to the median nerve at the wrist. Each patient received 800, 900, 1000, and 1100 shots from the first to the fourth session, respectively, at an energy density of 0.05 mJ/mm2 and a pulse frequency of 5 Hz. In the control group, all settings were applied but the start button was not pressed, so the machine produced the same sound without emitting any energy [22, 23].
Figure 1 depicts a flowchart of the participants throughout the study. There were no reported instances of adverse effects and no complaints were lodged during or after the treatment.
Outcome measures
Outcome assessments were carried out before the start of the first session and after the end of the last session after 4 weeks. The assessed variables encompassed Median nerve sensory and motor distal latency, arm volume calculated by circumference measurement, and assessing pain intensity by VAS as well as the Boston Carpal Tunnel Questionnaire (BCTQ). A physiotherapist conducted the assessment before and after the treatment.
Nerve conduction studies
An expert in physical medicine performed an electrodiagnostic assessment. Throughout the trial, the patients’ hand temperatures were maintained above 32 degrees. To evaluate the motor distal latency, an active recording electrode was secured to the abductor pollicis brevis (APB) muscle. A stimulator electrode was used to activate the median nerve at the wrist region, positioned 8 cm2 proximal to the active electrode. The sensory distal latency measurement involved securing the recorder on the third finger, then positioning the stimulator electrode 14 cm2 closer to the recorder. The median nerve was stimulated once at the wrist, in addition to once at the palm region, and the resulting distal latency was recorded. The patient had mild CTS if only the sensory distal latency was more than 3.6 ms, but moderate CTS if both the motor distal latency was more than 4.2 ms and the sensory distal latency was more than 3.6 ms and denervation was not detected on the electromyography of the APB [24].
Limb volume
Limb circumference measures were taken from the wrist dorsum to the axilla. This was done by taking a circumference measurement at each limb segment in between two successive circumferences. The volume of the segment can be determined via the formula V = h (C12 + C1C2 + C22)/12n, where V represents the volume of the segment, C1 and C2 represent the circumferences at the ends of the segment, while h represents the distance among them, which equals 10 cm in this case. A volume difference of 200 ml or more between the arms was considered to show lymphoedema [25].
Pain assessment (primary outcome)
The assessment was carried out using the Visual Analogue Scale, which is a valid and reliable tool for measuring pain intensity. It consists of a 10 cm line, where one end represents no pain, and the other end represents the worst pain. Each subject was requested to add a dot on the line that defines their pain level [26].
Boston Carpal Tunnel Questionnaire (BCTQ)
Patients with CTS can assess their level of dysfunction and symptom severity using the BCTQ. It has two measurement scales: the BCTQ-F, which measures the functional status and has 8 questions that are scored on a 5-point scale ranging from 1 (no trouble) to 5 (cannot accomplish anything due to hand or wrist symptoms) and is used to assess the degree of difficulty in carrying out daily function, and the BCTQ-S, which measures symptom severity and has 11 questions that assess the occurrence and severity of pain, numbness and weakness on a scale from 1 (no symptoms) to 5 (severe symptoms). The mean results of all questions are used to analyse the results [27].
Randomisation and blinding
Dependent variables were assessed at baseline and after four weeks by an assessor blinded to the treatment allocation. The computer-generated block randomisation method was used to assign the 68 female patients to either the study group that was given shock wave therapy along with the conventional physiotherapy program, or the control group that was given sham shock wave therapy along with the conventional physiotherapy program. To minimise the impact of selection bias and ensure consistency between the two sets of data, a block size of three was used. Opaque envelopes were sealed and numbered sequentially to accomplish the concealed allocation. The first author, who did not participate in data gathering, performed the randomisation. The second author unsealed the envelope and thereafter carried out the treatment based on the assigned group. The third author, who was unaware of the group allocation, performed the data collection at both the beginning and the conclusion of the intervention period.
Statistical analysis
The characteristics of the subjects were compared between the groups using an unpaired t-test. To compare the lymphoedema stage distribution among the groups, a chi- squared test was performed. To verify that the data had a normal distribution, the Shapiro-Wilk test was carried out. To ensure that the groups were alike, we used Levene’s test for homogeneity of variances. This study used an intention-to- treat analysis to assess the treatment effect on VAS, BCTQ, Sensory Nerve Distal Latency (SNDL) and Motor Nerve Distal Latency (MNDL), and in addition to limb volume, a two-way mixed MANOVA was carried out. Afterwards, we compared the results many times using post hoc tests that included the Bonferroni correction. A significance level of p < 0.05 was set for all statistical tests. Statistics were all performed using SPSS version 25 for Windows (IBM SPSS in Chicago, IL, USA).
Results
Physical characteristics of subjects
An unpaired t-test was conducted to compare the subject characteristics between groups. There were no significant differences between groups regarding age, weight, height, and BMI (p < 0.05). A chi-squared test was conducted to compare the lymphoedema stage distribution between groups and no significant difference was found (p = 0.40) (Table 1). The data was normally distributed and there was homogeneity between groups, which supports the use of parametric statistics.
Effect of treatment on VAS, BCTQ, SNDL, MNDL and limb volume
The effect of treatment was assessed using multiple outcome measures, including VAS, BCTQ, SNDL, MNDL, and limb volume. The result showed statistically significant improvements across all variables following the intervention.
Mixed MANOVA was conducted to determine the effect of the treatment on all variables in general, and it was found that there were significant effects of treatment and time (F = 29.59, p = 0.001). There was a significant main effect of treatment (F = 4.05, p = 0.002) and a significant main effect of time (F = 579.12, p = 0.001).
Within-group comparison
After treatment, compared to before treatment, there was a substantial reduction in VAS, Symptom Severity Scale (SSS), Functional Severity Scale (FSS), as well as limb volume for both groups (p < 0.001) (Table 2).
Table 2
Mean VAS, BCTQ and limb volume before and after treatment of experimental and control groups
There was also a substantial decline in SNDLand MNDL after treatment for both groups compared with that before treatment (p > 0.01) (Table 3).
Table 3
Mean SNDL and MNDL before and after treatment of experimental and control groups
Between-group comparison
The experimental group experienced a substantial reduction in VAS, SS and FSS compared to the control group following the treatment (p < 0.001). In contrast, the limb volumes of the groups did not differ substantially (p > 0.05) (Table 2).
There was also a substantial decline in SNDL and MNDL in the experimental group compared with that of the control group after treatment (p < 0.01) (Table 3).
Discussion
This study aimed to assess the impact of high-energy ECSWT on carpal tunnel syndrome in individuals with postmastectomy lymphoedema. Nerve conduction studies, limb volume, VAS and BCTQ were used a assessment methods. The outcome of this result after four weeks of intervention indicated decreases in the pain score in the study and control group by 3 cms and 2.12 cms respectively, SSS decreased in both groups by 10.78 and 7.19, respectively, FSS decreased by 7.29 and 4.57, respectively, and limb volume decreased by 166.75 ml and 153.46 ml, respectively. the SNDL decreased by 0.51 ms and 0.22 ms, respectively, and finally the MNDL decreased by 0.41 ms and 0.16 ms in the study and control groups, respectively, and found more benefit in the ECSW study group.
Extracorporeal shock waves are pressure waves that are created quickly and move faster than sound across the same medium. The biological consequences of the shock wave can be mostly attributed to a phenomenon known as acoustic cavitation. When applied, the waves release kinetic energy that can initiate tissue-reparative processes as they transfer a portion of this energy as they travel through tissues with various acoustic impedances [28]. ECSWT may have a reflexive analgesic effect by making axons more excitable and damaging unmyelinated sensory fibres [29]. The therapeutic effects include analgesic, osteogenic, and tissue-reparative effects that are mediated by various mechanisms such as the regulation of nitric oxide (NO), protein kinase B (PKB) and bone morphogenetic protein-2 (BMP-2) and transforming growth factor-beta 1 (TGF-p1) levels to promote osteoblast proliferation and differentiation [30]. Via vascular endothelial growth factor (VEGF), ESWT promotes the synthesis of endothelial nitric oxides (No), angiogenesis, and neurogenesis. ESWT also has anti-inflammatory properties in addition to reducing calcitonin gene-related peptide (CGRP) in the soft tissue around the median nerve. Pain is relieved following treatment because of the quick degradation of intracutane- ous nerve fibres that occurs after applying ESWT [8].
The advantages found in the ECSWT group may be attributed to the biological effects of ECSW, which include angiogenesis, bone remodelling, tissue regeneration, wound healing, and an anti-inflammatory effect [31]. The biological benefits of extracorporeal shock wave therapy (ESWT) have been proposed to be due to mechanotransduction, a process that depends on ultrasonic vibrations acting on tissues to promote healing and regeneration [32]. ESWT’s anti-inflammatory effects are typically similar to the mechanisms of action seen in other musculoskeletal disorders for which it is frequently prescribed [33]. A study by Mittermayr et al. showed that ECSWT has anti-inflammatory effects by increasing NO levels through both enzymatic and non-enzymatic NO generation [34]. The release of nitric oxide may therefore stop the inflammatory process from being induced by lipopolysaccharide and interferon-gamma production. At this point, two main theories have been put forth to account for the analgesia brought on by ECSW therapy. One proposes that the shock waves reduce the concentration of pro-inflammatory mediators by degenerating nerve fibres from tiny immunoreactive neurons. The second process involves hyperstimulation, selective destruction of sensory unmyelinated fibres within the focal zone of the applied shock wave, which suggests that shock waves activate the descending inhibitory system, which in turn releases endorphins and other analgesic chemicals, causing analgesia [35].
The results of this study are consistent with those of previous research [36-38]. The application of ESWT in patients with CTS has increased significantly and proven its therapeutic benefits. Between 2018 and 2020, a cross-sectional descriptive study included 320 patients with postoperative lymphoedema in Iran’s hospitals affiliated with Tabriz Medical University. Participants were identified using the BCTQ, and the chi-square test was used to investigate the data. 20% of the patients reported CTS symptoms in the questionnaire. Data analysis showed that diabetes, radiation therapy and surgical removal of lymph nodes could contribute to the development of CTS. The outcomes revealed that one in five women who underwent chemotherapy and had lymphoe- dema after mastectomy experienced CTS symptoms [39].
To relieve pain, neuronal NO synthase (nNOS) is produced during ESWT. NO can replace opioids. This eliminates the need to bind to opioid receptors. In this case, the hyperpolarised nerve may have lower excitability even with reduced pain, leading to less improvement in the NCS parameters [36]. In a study by Ke et al. [8], ESWT was performed once per week using 2,000 pulses at a pressure of 4 bar and a frequency of 5 Hz, targeting the median nerve from the level of the pisiform bone to the proximal end of the carpal tunnel. The researchers determined that ESWT was a potentially effective treat ment approach for those with mild-to-moderate CTS, and that many sessions of ESWT resulted in cumulative clinical outcomes. Seok and Kim [40] also proved that in individuals with mild-to-moderate CTS, just one session of SWT can be equally advantageous as a local corticosteroid injection in decreasing subjective symptoms. Our findings corroborate previous research showing that mild-to-moderate CTS patients can benefit from three sessions of ESWT, with decreased pain and disability compared to ultrasound as well as cryo-ultrasound therapy, and that these benefits can persevere for months [41].
Research by Raissi et al. [42] asserted that a study including radial ESWT and a splint among patients having mild to severe CTS demonstrated no statistically significant difference in pain intensity or Boston Questionnaire (BQ) score among groups. However, both groups exhibited a notable improvement in their scores when treated with ESWT and a splint or a splint alone. Statistical analysis of the Raissi trial found that a splint alone was more effective than ESWT with a splint at reducing pain intensity and BQ scores. As the shockwave is dose-dependent, the researchers blamed these outcomes on the lack of an acceptable treatment dose, which includes the quantity of sessions and shocks. Low-energy ESW has been documented in the literature as a secure and efficient treatment approach for nerve tissue [43]. In addition, peripheral nerves are not affected by high-energy ESWT. In addition to CTS, ESWT is employed for the treatment of peripheral neuropathies, including distal symmetric polyneuropathy as well as interdigital neuroma [44]. Moreover, some investigations have demonstrated that ESWT exhibits antiinflammatory effects by augmenting nitric oxide (NO) levels via both non-enzymatic and enzymatic NO synthesis. The antiinflammatory effects of this substance can alleviate carpal tunnel inflammation, which lowers the perineural pressure and providing relief from discomfort [45]. The outcomes of the study performed by Xu et al. [37] showed that in individuals with mild to severe CTS, three sessions of low-energy radial ESWT resulted in a substantial reduction in the sensory latency of the distal median nerve throughout the 9- and 12-week follow-up assessments. Two current meta-analyses by Kim et al. [45] as well as Xie et al. [46] found that ESWT may help CTS patients with their symptoms, functional outcomes, and electrophysiological characteristics.
Limitations
The study was constrained by two factors: the psychological and physical condition of the patients throughout the treatment duration, as well as the small size of the sample. Additional measuring tools may be required to ensure optimal reliability. Examining the long-term results is crucial for evaluating the effects of the treatment methods. The limitations of this study were that there was no follow-up because some of the participants forgot the follow-up time, transport problems, and others thought that the follow up was not essential.
Conclusions
The outcome of this study showed a reduction in pain, improvements in the sensory and motor distal latency of the median nerve, and improved functional status in both groups, with more benefits in the group that received ECSWT.
Recommendations
Based on the latest research, it is recommended to explore using ESWT as a safe and effective non-invasive treatment for reducing pain and the severity of symptoms in CTS associated with postmastectomy lymphoedema. However, further research and alternative assessment methods are required to examine the impact of ESWT on CTS among those with postmastectomy lymphoedema.