Introduction
Shoulder impingement syndrome (SiS) is defined as pinching of soft tissues of the subacromial space (supraspinatus and long head of biceps tendons, and the bursa) between the humeral head and acromion during arm elevation causing marked pain and disability [1]. SiS is the cause behind 3638.6% of shoulder painful pathologies and affects 5-47% (1-year prevalence) of the population (commonly aged 2540 years) in Egypt and globally [2-4]. The international Classification of Diseases (iCD-10) coded SiS as M75.4 [5].
Sis has 3 stages; phase i affects young persons (< 25 years) and is characterised by oedema/haemorrhage and treated non-operatively, phase ii affects those aged between 25 and 40 years, is characterised by fibrosis/tendinitis, and is treated non-operatively or with debridement, and the last phase affects older subjects, is characterised by bone spurs and tendon rupture, and is treated by decompression and/or repair [6]. Common causes/risk factors include muscle ro tator cuff and scapular muscle weakness/imbalance, capsular tightness, poor posture, overuse, and bony ingrowth [7]. Common non-operative interventions include medications, in- tra-articular injections, and physical therapy (mobilisation, rotator/scapular strengthening, capsular stretching) [6, 8].
The cervical spine is a key area of proprioception, which maintains normal alignment of body segments, functional stability, and controlled mobility for the cervical, scapular, and shoulder regions [9-11]. Cervical proprioception and posture are impaired in SiS [12, 13], leading to shoulder muscle fatigue, altered mechanics, and functional instability [14]. As a consequence, shoulder impingement commences [15].
Rehabilitation and exercises are effective in treating shoulder pain [16, 17]. However, SiS has a high recurrence rate, recurring in about 16% of patients within 2 years of proper rehabilitation [18]. it is hypothesised that impaired proprioception and postural control may be the cause behind this recurrence. This suggests further investigations in the rehabilitation of SiS, such as proprioceptive training [19, 20]. Zedan et al. [20] found that strengthening of the deep neck muscles (which improves cervical proprioception due to their richness in muscle spindles) improved shoulder proprioception in SiS patients. This is important for patients with SiS as they showed poor proprioception [19]. Directly targeting cervical proprioception via cervical proprioceptive training (CPT) is hypothesised to improve shoulder proprioception more. However, there is a lack of studies addressing the effect of cervical proprioceptive training (CPT) on shoulder proprioceptive error, pain, and dysfunction in patients with SiS. investigating the effects of CPT in treating SiS may help physiotherapists to deal with and treat SiS patients in the period of acute or subacute symptoms, where improving shoulder symptoms by active and resistive exercises is not applicable or restricted.
Almost all studies addressed effects of CPT on neck posture, proprioception, and pain and found positive results. No studies related to SiS were identified by the researcher [21,22].
Therefore, exercises specifically targeting individual muscles with low intensity may not be sufficient to improve shoulder joint position sense in healthy subjects. Future work is needed to further investigate which types of exercise are more effective in improving joint position sense, and the mechanisms associated with those changes [23].
Determining the effects of cervical proprioceptive training in treating SiS may help physiotherapists to deal with and treat SiS patients in the period of acute or subacute symptoms, where improving shoulder symptoms by active and resistive exercises is not applicable or restricted. There is a lack of studies addressing the effect of cervical proprioceptive training on shoulder outcomes (proprioception, pain, function) in SiS patients.
Therefore, this study was conducted to study the effects of ‘cervical proprioceptive training’ on shoulder proprioception, pain, and disability in patients with SiS.
Subjects and methods
A ‘randomised controlled, parallel group trial’ was performed at the 23rd of July Chest Hospital in El-Marg, Egypt, from January 2023 until May 2024.
Participants
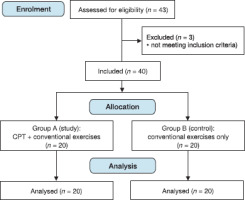
Forty patients with SiS diagnosed by an orthopaedist (5 years of experience) and rechecked for SiS criteria by the researcher. Patients were randomly and allocated (1:1 ratio) into two groups: group A received CPT plus conventional exercises (scapular and rotator cuff strengthening exercises, and posterior capsule stretching), while group B received conventional exercises only. Randomisation was performed using the simple method of closed envelopes with sequentially numbered containers for allocation. A subject not otherwise associated with this research randomised and allocated the patients, and the researchers did not know the allocated group of any patient before the baseline assessment. The sample size was determined by the G*power software using an effect size (d) = 1.3 for shoulder internal rotation proprioception from a previous study [15], power 0.95, and significance 0.05.
Patients were included if they had SiS (based on criteria reported elsewhere [24]), age range between 25 and 40 years, and BMi < 32 kg/m2. Patients were excluded if they had: osteoarthritis, rotator cuff tear, trauma, infection, intra-articular injection within the last 3 months, surgery to the shoulder, or symptomatic cervical pathology.
Procedure
Assessment procedure
Each patient signed an informed consent form before starting the study. Then, all subjects were evaluated for their shoulder pain, disability level, and proprioception before and after the four weeks of the treatment program.
Shoulder pain and disability were measured using the Shoulder Pain and Disability index (SPADi). it is valid (moderate to strong), reliable (high; iCC = 0.87-0.96) and highly responsive in assessing shoulder pain (5 items) and function (8 items). The minimal clinically important difference (MCiD) values for SPADi-pain, -disability, and -total were reported as 3, 13, and 14-20, respectively [25-28].
Proprioception: The Protractor smartphone App was used for assessing shoulder active joint angular reproduction error during shoulder iR and ER at 30° (reference angle). it had acceptable reliability (iCC = 0.7-0.94) and validity (iCC = 0.60.72) [29]. Firstly, the affected shoulder of the patient was put in 30° abduction and horizontal adduction, and 90° elbow flexion. Next, the shoulder was passively moved and positioned at the reference angle by the researcher and held for 10 seconds with opened eyes. The arm was then passively returned to the starting position. The subject was instructed to actively reposition the shoulder at the reference angle and hold for recording with closed eyes. Three trials were recorded and averaged as the absolute difference in degrees between the patient’s arm angle and the reference angle [30]. MCiD was reported as 2.5 [31].
A laser pointer was used for assessing cervical proprioception. it had good reliability (r = 0.68) and validity (r = 0.95) [32]. The patient sat with the back supported and head free to move. A target piece of paper was fixed on a wall about 90 cm from the seat and at a distance from the ground adjusted for the height of the patient. A laser pointer was strapped to the highest point of the head of the patient, who was instructed to move their head in the tested direction (flexion and extension, and right and left rotation), then fix the laser beam back on the centre of this piece of paper for 10 s while keeping the eyes open. The point reached in each direction was marked. Then the distance between the piece of paper’s centre and the reached point was measured using a tape measure [33, 34].
Treatment procedure
Treatment included three sessions of 20-30 min weekly for four weeks. Patients were instructed not to use medications for pain relief unless necessary and should tell the researcher.
Cervical proprioceptive training (CPT)
The patients of group A received CPT through the use of a laser pointer in a similar way to the testing. From a sitting position, the patients were asked to flex, extend and rotate their head and then return it to the neutral position (Figure 1A). This training was commenced with open eyes. Each direction was repeated 8 times for two sets, with 30 s rest between sets. Progression was achieved by closing the eyes and altering the duration (trace shapes for 5 min and progress by increasing by 2-3 min weekly as tolerated), repetitions (2-3 repetitions weekly), sets (1 set weekly) and the degree of difficulty of the task (different shapes and positions, such as standing and walking) [35-37].
Conventional exercises
Patients of both groups received shoulder posterior capsule stretching exercises (Figure 1B) (cross body and sleeper stretches) (Figure 1C), scapular stabiliser strengthening exercises (Figure 1D, E), and proprioceptive neuromuscular facilitation diagonal 2 flexion (PNF D2F) (Figure 1F) as described elsewhere [7, 38-42]. Each stretching exercise was performed three times for 30 min with a 10 s rest interval, whereas each strengthening exercise was performed for 3 sets of 10 repetitions, with 3-5 s hold, 3-5 s rest between repetitions and 20 s rest between sets.
Statistical analysis
Statistical analysis was conducted using SPSS for windows, version 24 (SPSS, inc., Chicago, iL). The alpha level was set at 0.05. The data did not significantly violate the normality assumption (p-value > 0.05). Homogeneity of variance was satisfied (p-value > 0.05) and measured using Levene’s test. Differences between groups in continuous and categorical demographic variables were determined using the independent t-test and Chi-squared test (likelihood ratio was used in case of violation of assumption), respectively. Analysis of covariance (ANCOVA) with pre-test scores as covariates was used to test differences between group, whereas the paired t-test was used to test differences within groups. Correlations between cervical proprioception and outcomes were measured with Pearson’s correlation coefficient (r < 0.39 is a weak correlation, r = 0.40-0.69 is moderate, r = 0.70-1 is strong/ high) [43].
Results
The number of patients who were enrolled, randomised, treated and analysed are shown in Figure 2. One patient from each group crossed over to the other group. intention-to-treat analysis was applied, and the patients were analysed as assigned. There were no drop-outs or adverse events, given short treatment duration and simple program. All patients attended at least 70% of the sessions.
General characteristics
Table 1 shows the baseline characteristics of the patients in both groups. There were non-significant differences in the baseline characteristics between groups (p > 0.05).
Table 1
Baseline characteristics of the two groups
Effect of CPT on shoulder pain, function, and proprioception
Within-group differences
There was a significant decrease in shoulder pain (p-value, 95% Ci, and effect size were < 0.001, 16.2-23.1, and 3 for group A, < 0.001,9-19, and 1.3 for group B) and disability (p-value, 95% Ci, and effect size were < 0.001,20.4-29.8, and 1.7 for group A, < 0.001,9.7-23.5, and 1.13 for group B) at post-treatment in both groups. Moreover, there was a nonsignificant decrease in shoulder proprioceptive error (at external rotation) at post-treatment in both groups (p > 0.05) but group A had a trend towards significance (p-value = 0.07, 95%: -0.14 -2.3, d = 0.46 vs. 0.25). While, for internal rotation, there was a significant decrease in shoulder proprioceptive error at post-treatment in group A only (p = 0.01, 95% Ci: 0.33-2.18, d = 0.69 vs. 0.29) (Table 2).
Table 2
Shoulder pain, disability, and proprioceptive error within and between groups
Between-group differences
There were no significant differences between groups in shoulder pain and disability at post-tests (p > 0.05) using ANCOVA with pre-test values as covariates. Moreover, there was a significant difference between groups [p-value = 0.03, 95% Ci: -3 to -0.1, effect size (partial eta squared): 0.12] for internal rotation only (Table 2).
Correlations between cervical and shoulder proprioception
Table 3 shows that cervical (left rotation) and shoulder proprioception (iR) values were moderately correlated (r = 0.49, p-value < 0.01) only in the study group. There were also moderate correlations (r = 0.59 and 0.58, respectively) between cervical flexion proprioception and shoulder pain and disability (p-value < 0.01), also only in the study group.
Table 3
Pearson's correlation coefficients (r) between cervical and shoulder proprioception
Discussion
The present trial aimed to study the combined effects of CPT and conventional exercises on shoulder pain, disability, and proprioception in shoulder impingement syndrome patients, compared to conventional exercises alone. The study showed that both groups improved significantly post-treatment (p < 0.05) in shoulder pain and disability, while shoulder proprioception (internal rotation and a trend in external rotation) improved in group A only. Moreover, cervical and shoulder proprioception values were moderately correlated. Effect sizes were large in both groups regarding pain and disability but were higher in the study group, whereas proprioception was only moderate-to-large in the study group versus small in the control group. This and the relatively small Ci indicate the strong clinical significance of CPT in improving shoulder proprioception in SiS patients.
Improved pain in both groups can be explained by the effects of the proprioceptive and/or resistive exercises (dynamic and eccentric contraction of the muscles) on inducing local and global hypoalgesia through endogenous pain modulation [44].
Cpt improved cervical and shoulder proprioception significantly, rather than shoulder function. This finding is supported by the work of Ozudogru et al. [45], who reported that there was no relation between shoulder function and cervical proprioception in healthy young subjects. This may be due to only healthy young subjects with no/little differences and/ deficits in the studied variables being included.
In 2022, Fatima et al. [46] investigated the effect of adding shoulder proprioceptive training to cervical stabilisation exercises for 4 weeks on neck pain, disability, and proprioception in 28 chronic neck pain patients aged 18-45 years. The authors found additional improvement in pain, disability and proprioception [46]. in the present study, we investigated the effect of adding cervical proprioceptive training to shoulder stabilisation exercises on shoulder pain, disability, and proprioception in 40 SiS patients aged 25-40 years and found increased improvement in shoulder proprioception. However, while the difference in the studied populations, small sample size, and short treatment duration might reduce the significance of other (subjective) variables, the significant improvement in shoulder proprioception is an interesting finding because patients with various shoulder pathologies, including SiS, demonstrated increased proprioceptive errors [47]. Moreover, higher proprioceptive errors in SiS were related to the level of shoulder disability and pain [19]. in the present study, shoulder proprioception improved significantly with no significant reduction in pain and disability, which can be explained by the short treatment duration and small sample size.
The CPT improved the posture and balance [48], therefore increasing the treatment duration may improve the efficacy of CPT in reducing pain and disability by improving poor posture, which can cause shoulder symptoms and their recurrence as well. Proper proprioception and postural control may improve the fine control of movement and prevent microtrauma to the tissues during normal daily movement. Positive effects from proprioceptive and stabilisation training might be induced by several mechanisms, such as normalised muscle firing/activity and improved blood circulation [49].
Ager et al. [50] found that adding shoulder proprioceptive training to the conventional program improved shoulder proprioception, but not pain and disability, over the conventional program alone in SiS patients. Merging this finding with the findings of the current study may suggest that, in the early stage of rehabilitation of SiS, where the pain/symptoms may limit application of shoulder proprioceptive training, the application of CPT represents a safe and effective alternative solution.
As with previous studies [51,52], shoulder stabilisation exercises (SSEs, e.g. stretching capsule, strengthening cuff/ scapular muscles) improved shoulder pain and disability in 20 healthy subjects [51] and 60 patients with shoulder pain [52]. However, shoulder proprioception did not improve in the control group in the current study (received SSEs) compared to previous studies. This difference may be further explained by the shorter training duration and methodological differences in the present study compared to previous ones.
Besides its high effectiveness, CPT has no adverse effects as no patients reported any harm, took any medication after the sessions due to adverse reactions, or dropped-out.
This study should be taken with its limitations, which include the short period of treatment and lack of a placebo or sham control group. in addition, not all patients progressed to the advanced levels of CPT.
Conclusions
Conventional exercises with or without cervical proprioceptive training improve shoulder pain and disability, but they did not improve shoulder proprioception alone in patients with SiS. Future studies need to investigate effects of cervical proprioceptive training in treating athletes with atraumatic, non- structural instability.