Introduction
Axillary web syndrome (AWS) can develop after axillary dissection surgery (AdS) and is characterised by the extension of cords of subcutaneous tissue from the armpit into the arm. AWS can cause pain and restrict shoulder mobility in the affected arm. The disorder is always self-limiting and may occur early or late post-surgery [1].
AWS is often caused by injury to the axillary lymphatic system during surgery, but the exact pathophysiology is not fully understood. Some evidence from echography and magnetic resonance imaging suggests it is related to lymphatic damage [2]. AWS is usually diagnosed by physical examination, and risk factors include the extent of surgery, younger age, hypertension, lower body mass index, origin, and complications during healing [3]. The condition is considered a risk factor for lymphedema due to similar pathophysiology.
Effective clinical intervention can shorten the expected course of AWS and modify patient quality of life [4]. Treatment options include physical therapy, drug therapy, instrument-assisted soft tissue mobilisation (iASTM), thoracic manipulation and stretching, manual axial distraction, transcutaneous needle cord disturbance with fat grafting, Xiaflex injection, and surgical intervention [5]. Additionally, AWS treatment may involve active and passive stretching and cord stretching methods such as myofascial and scar release [6]. depending on a patient’s acuity and presentation, different manual approaches are used. The most helpful method is thought to be skin traction, where the therapist’s thumb and index finger stretch one or 22-inch portions of the cord while the arm is abducted to a comfortable level and can be applied to the chest wall and the entire length of the cord [7]. The therapist may occasionally feel the cord pop or snap when it breaks during the stretch. in most cases, the patient experiences no pain and immediately gains more range of motion (RoM). Rather than the thickened cords observed in the axilla, this therapy frequently results in thinner piano-wire-type cords in the antecubital fossa and down the length of the cord [8].
Radial shockwave therapy (RSWT) has been used for many years to treat myofascial pain. Recent studies have shown promising results when combining low-energy extracorporeal shock wave therapy (ESWT) with complex decongestive therapy in patients with breast cancer-related lymphedema (BCRL), leading to improved RoM in the shoulder joint and skin thickness improvement. Given these positive outcomes, researchers are now exploring the potential application of RSWT in patients with AWS to enhance RoM and alleviate pain [9].
Recommending an appropriate treatment plan to lessen the negative psychological and physical impacts of AWS treatments remains a challenge, and diagnosis and treatment of the disorder require further research. Therefore, the current study investigated the combined effects of RSWT and a tailored exercise program (TEP) on AWS after breast cancer surgery with AdS.
Subjects and methods
The study was a controlled, double-blinded, randomised clinical trial (participants and assessors were successfully blinded to the group allocations) carried out at The damietta Cancer institute between June 2022 and december 2022. Clinical applications of RSWT, TEP, and patient physical assessments were undertaken at the outpatient clinic, Faculty of Physical Therapy, delta University for Science and Technology. After AdS for breast cancer, a surgical oncologist diagnosed all patients with visible and/or palpable AWS and referred them to physical therapy. Patients who met the inclusion criterion of being female and between the ages of 40 and 65 were enrolled. Patients were not eligible if they had metastases of any kind, lymphedema, a traumatic injury to the targeted upper extremity, a musculoskeletal disorder, were taking any anticoagulants, had undergone bilateral breast cancer surgery, experienced locoregional recurrence, or had vascular problems in the affected upper extremity. Participants were also excluded if they declined to take part or sign the written consent form. The sample size was calculated using G*Power (dusseldorf, Germany) to find a difference of 50% of shoulder RoM (flexion and abduction). The calculation used a confidence interval of 95% and a margin of error of 5%. Using these criteria, the estimated sample size for each group was 29 patients, and this number was increased by 15% (35 patients) to account for any dropouts between the time of randomisation and the end of the treatment protocol.
Patients were randomly assigned to receive RSWT and TEP (group A), RSWT only (group B), or TEP only (group C). The study employed block randomisation by using a computer-generated table of random numbers concealed within sealed opaque envelopes, which serves to reduce potential imbalances in participant allocation, thereby enhancing the statistical validity of the study outcomes. The concealment of the randomisation categories within sealed envelopes acts as an additional safeguard against bias, ensuring the integrity of the allocation process. The patient’s shoulder RoM, pain intensity, upper extremity activities, echogenicity, thickness, and disorganisation were assessed using a digital inclinometer, visual analogue scale (VAS), an abbreviated disabilities of the arm, shoulder and hand (Quick dASH) assessment, and diagnostic ultrasound, respectively. The stratified randomisation process was overseen by a professional physical therapist who was not involved in the study procedures.
The outcomes were collected by a well-experienced investigator blinded to the group assignments and considered as part of the research team.
Assessment measures
According to Kolber et al. [10], a digital inclinometer is a reliable tool for measuring shoulder RoM. The inclinometer was placed near the shoulder at the proximal area, and with the patient’s feet fixed, they moved their shoulder in different directions (flexion and abduction). The examiner repeated the measurements three times and recorded the mean value.
Pain intensity was measured using the VAS. Using a continuous 100 mm horizontal line beginning on the left side with no pain and ending on the right side with more pain, the patients marked the VAS point that corresponds to their pain level. The researcher then determined a score between 0 and 100 mm by measuring the distance (mm) on the line between the patient’s mark and the “no pain” sign on the left side [11]. The measurements were taken at the start of the study as a baseline and 4 weeks after the interventions.
The Arabic version of Quick dASH is a reliable and valid measure for assessing disabilities in the upper extremities of Arabic-speaking populations, with Cronbach’s alpha (0.89) indicating good internal consistency and intraclass correlation coefficient (iCC) (0.94) suggesting good test-retest reliability [12]. The measurements were taken at the start of the study as a baseline and 4 weeks after the interventions.
An ultrasonography technique involving a high-resolution ultrasound system with 18 MHz frequency provided high-definition superficial imaging that allowed measurement of cord thickness, echogenicity, and disorganisation [13]. A gel was used to reduce artefacts caused by tissue compression. The measurements were taken at the start of the study as a baseline and 4 weeks after the interventions.
Treatment procedures
Radial shock wave
The patient lay supine with the affected shoulder in an abducted position to expose the axillary cords. Each patient received 3000 shocks to different areas, including 1000 to the axillary, 500 to the upper arm, 1000 along the course of the cords, and 500 to the antecubital space. Pneumatic ESWT (EME Srl, Pesaro, italy) was administered over two sessions during the first 2 weeks of the intervention and one session each in the third and fourth weeks. The shocks were delivered using an auto-continuous mode at 3 bar and 12 Hz, with individual shocks of 0.432 joules equating to 1296 joules per session.
Tailored exercise program
The standard exercise session consisted of a warm-up of 60 small arm swings performed for 5 min. Each stretching exercise was then executed for 2.5 min, followed by a 2.5-min rest period. The entire exercise session lasted 45 min. After completing the session, there was a two-hour rest period before repeating the exercises. Subsequently, the exercises were integrated into a home care program, with a frequency of twice a week for four consecutive weeks. The TEP involved snow angels, butterfly wings, forward pinky slides, corner stretches, chest stretches, self-tissue stretching, overhead moose stretching, and crescent side bends (Table 1).
Table 1
Description of exercises (TEP)
Statistical analysis
Statistical analysis employed SPSS software for Windows, version 21.0 (iBM Corp., NY, USA). The data were used to generate descriptive statistics for the three groups at baseline and 4 weeks after treatment. Homoscedasticity was assessed using Bartlett’s test before statistical analysis to determine the suitability of parametric testing. The Shapiro– Wilk test determined data distribution, while one-way analysis of variance (ANoVA) evaluated the homogeneity of groups by comparing the baseline data for age, weight, height, body mass index (BMi), arm length, cord length, VAS, active shoulder flexion, active shoulder abduction, and cord thickness. The chi-squared test analysed the distribution of data for the disorganisation and echogenicity results. one-way ANoVA with post hoc Tukey tests compared the three groups after 4 weeks of treatment for VAS, active shoulder flexion, active shoulder abduction, and cord thickness. The interquartile range analysis detected the median values for disorganisation and echogenicity at the baseline and after 4 weeks of treatment within each group. The Kruskal–Wallis test determined the p-values for the median disorganisation and echo-genicity values within groups. A p-value of less than 0.05 was set as the threshold for statistical significance.
Results
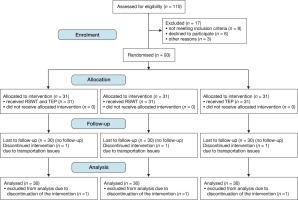
AWS patients (n = 110) who underwent breast cancer surgery with AdS were recruited from the damietta Cancer institute. Patient eligibility was assessed by a surgical oncolo-gist at the outpatient clinic of the Faculty of Physical Therapy, delta University for Science and Technology. Eight patients did not meet the inclusion criteria, six declined to participate, and three were excluded for other reasons. The patients were then referred to physical therapy. Figure 1 illustrates the patient flow diagram.
The remaining 93 eligible patients were randomly assigned to one of the three groups. Three patients (one from the combined therapy group, one from the RSWT group, and one from the TEP group) could not complete the study due to transportation issues.
No adverse effects of the treatment protocol were reported in any of the groups, according to the feedback provided by the patients. The baseline data for all bio-demographic and clinical characteristics, such as age, weight, height, BMi (body mass index), arm length, shoulder flexion and abduction, VAS, cord length, thickness, echogenicity, disorganisation, length, and Quick dASH, did not show any statistically significant differences between the groups (Tables 2 and 3).
Table 2
The Baseline characteristics of patients in groups A, B, and C
Table 3
Baseline characteristics of cord organisation and echogenicity for groups A, B, and C
The results showed that the mean values of VAS, shoulder flexion and abduction, cord thickness, and Quick dASH were significantly different between baseline and after 4 weeks of intervention (p < 0.05) (Table 4).
Table 4
Comparison of variables across groups A, B, and C before and after treatment
When analysing the mean differences and 95% confidence intervals for various outcome measures (shoulder flexion and abduction, VAS, cord thickness, and Quick dASH) across the three, the findings indicated that group A exhibited higher values than group B. Additionally, group C demonstrated lower values than groups A and B. Notably, the results indicated non-significant differences between groups B and C across most of the compared variables, as evidenced by the F-statistics and p-values in Table 5.
Table 5
Comparison of mean differences, 95 % confidence intervals, degrees of freedom, F-statistics, and p-values for shoulder flexion and abduction, VAS, cord thickness, and Quick dASH across groups A, B, and C
[i] VAS – visual analogue scale, F-statistic – F = MS between/MS within, where MS between is the mean square between groups and MS within is the mean square within groups Mean differences, confidence interval (95 %), degrees of freedom, F and p-values were obtained using one-way analysis of variance with post hoc Tukey tests.
When measuring the interquartile range of cord disorganisation and echogenicity at baseline and after 4 weeks of intervention, the results showed statistically significant differences among the three groups, with higher percentages of improvement in group A compared to B and C (Table 6).
Table 6
Interquartile range of disorganisation and echogenicity
Discussion
The study investigated the effectiveness of RSWT, TEP, and combined therapy (LESW and TEP) in treating AWS in breast cancer patients following AdS. No negative effects were reported for any of the treatment protocols in any of the three groups.
The baseline demographic and clinical data showed no significant variation between the groups. However, after 4 weeks of intervention, the mean differences in VAS, shoulder flexion and abduction, cord thickness, and Quick dASH were significantly differences between the groups. Specifically, group A had higher values than group B and lower values than group C. in addition, the interquartile range of cord disorganisation and echogenicity varied between the three groups, with maximum improvement observed in group A, followed by group B and group C.
The findings suggest that RSWT combined with TEP may be effective for treating AWS in breast cancer patients following AdS. However, group A seemed to have higher improvement rates than the other two groups, indicating the potential for further optimisation of treatment protocols to improve overall patient outcomes.
A prospective clinical trial by Bae and Kim [14] with a small sample size of seven participants compared the effectiveness of RSWT on breast cancer-related lymphedema with and without lymphatic massage. The authors described the trial’s constituent elements, including study population characteristics, ESWT setting parameters, and methods of clinical outcome measurement evaluation. Both groups showed marked improvement in the measured outcomes, including upper extremity volume, circumferences, and skin thickness, but no significant difference was found when comparing the two groups [14].
The current study has important clinical implications, as AWS can substantially impact the quality of life of breast cancer survivors. As such, RSWT and TEP could offer a safe and effective treatment option for AWS symptoms.
Based on a search for studies that are parallel to or contradict our study on the combined effect of RSWT and TEP on AWS after mastectomy with AdS, a study published in 2022 investigated the effectiveness of RSWT for breast cancer-related lymphedema. The study found that RSWT significantly reduced the affected limb’s volume and improved symptoms compared to the control group. The findings of this study are in agreement with our work and demonstrate the potential effectiveness of RSWT in improving symptoms related to breast cancer surgery [15].
Consistent with the existing literature, we found that AWS can be triggered by various factors, including radiation therapy and specific types of breast cancer. Previous studies have shown that RSWT can induce positive effects such as pain relief, angiogenesis, protein synthesis, cell proliferation, nerve and cartilage protection, and disruption of calcium deposits in musculoskeletal structures [16–18]. These combined effects have the potential to promote tissue regeneration, provide significant pain relief, and enhance the functionality of damaged tissue [19–23]. our study involved stretching exercises designed to improve RoM and reduce tension in the affected area. Physical therapy, including stretching exercises, is a widely used treatment option for AWS, and our research supports its effectiveness. in summary, our controlled clinical trial explored the potential of ESWT and TEP in managing AWS following breast cancer surgery with AdS. We observed promising outcomes in terms of pain relief, improved RoM, and functional improvement in the damaged tissue. However, further research is needed to validate these findings and establish optimal protocols for ESWT and TEP use in AWS management.
Limitations
Limitations of the current study include the lack of a placebo control group. Since all participants received some form of treatment, it is challenging to determine if the improvement was due to the treatment itself or simply the passage of time. Additionally, the short follow-up period could not detect any potential long-term benefits or adverse effects of the treatments being tested. Another limitation is the heterogeneity of the study population, as the effectiveness of treatments may vary depending on the severity of the condition. Therefore, future studies with longer follow-up periods are needed to confirm the efficacy of this intervention and its long-term effects. Recommendations for future studies include increasing the diversity of participants, as this can improve the generalisability of the findings. Additionally, using a placebo control group can accurately assess the effectiveness of the interventions, while a longer follow-up period can provide insights into any potential long-term benefits or adverse effects of the treatments. Conducting stratified or subgroup analyses based on the severity of the condition or other relevant demographic or clinical factors can also help evaluate the interventions’ efficacy.