Introduction
Adolescent idiopathic scoliosis (AiS) is a three-dimensional deformation of the spine. Severe deformities have the potential to diminish the volume of the rib cage, hinder the mobility of the ribs, and leave respiratory muscles at a mechanical disadvantage [1].
Participants undergoing thoracic cage surgical interventions to help manage their AiS experienced significant alterations in their anticipated lung functional values for up to five years after surgery. it has been suggested that these values can be maximised following surgical treatment of scoliosis [2].
Modifications in chest compliance can lead to impaired pulmonary function. in severe deformities, limitations in achieving appropriate ventilation-perfusion and airway obstruction have adverse consequences for respiratory function [3].
Jasiewicz et al. [4] proposed the potential improvement of post-operative deteriorational surgery on respiratory muscular strength in those suffering from AiS, particularly among those who have undergone anterior surgical intervention.
Therefore, a well-designed pre-operative rehabilitation program focusing on pulmonary issues is a crucial component for such individuals to accelerate post-operative improvement, which minimises the negative impact on a patient’s quality of life.
The evaluation of cardiopulmonary functions should be a component of the clinical evaluation for AiS, mainly for those who have greater Cobb angles. in addition, children with AiS should undergo post-operative assessment of their cardiopulmonary function [5].
More research is required to enhance the quality of evidence. Prospective clinical trials are needed to determine the temporal relationship of corrections in spinal/thoracic issues and pulmonary functional alterations to guide optimal AiS management, particularly for those who are at risk of breathing difficulties [6].
We hypothesised that vertebral derotation would improve pulmonary function and mechanical parameters following the surgical treatment of AiS.
Subjects and methods
Subjects
A total of sixty participants were selected to participate in the current prospective study, with four individuals being omitted from the analysis due to various reasons. A total of 56 participants, comprised of 10 males and 46 females, who suffer from AiS with a single thoracic curvature, were allocated into two equal groups using blocked randomisation. Prior to their involvement, all patients underwent a clinical examination conducted by a chest physician to rule out the presence of any pulmonary, cardiac or vascular conditions that could potentially impact pulmonary function.
Surgery was advised for AiS after a certified spinal surgeon’s diagnosis following a complete clinical and radiological evaluation that includes Cobb and rotational angle measurements. Patients over the age of ten having no other conditions that could influence the test’s outcomes were included in the study. A parent or legal guardian’s written permission was required for participation in the study. No physical treatment was utilised by the participants before the operation.
Curvatures larger than 40 degrees using Cobb’s technique or a progressive Cobb angle greater than 5 degrees at the three-month follow-up were recommended for surgery. deterioration of such scoliotic curvatures leads to negative deteriorations in pulmonary function that might lead to complete respiratory failure [4, 5].
We positioned the involved participant in prone using a Jackson’s operative table. over the levels to be combined, a midline incision is made, and the posterior elements are cautiously exposed to the transverse process tips. The inferior dorsal facets were osteotomised using a small osteotome to regain axial flexibility and exposed to the superior articular facet. The superior dorsal facets were exposed to enable full excision of cartilaginous portions to gain perfect fusion and to serve as reference points for the placement of thoracic pedicle screws [7].
Participants were allocated into two equal groups, each containing 28 AiS patients. Group A (derotation group, dRG) received a vertebral derotation technique during posterior correction and post-operative pulmonary rehabilitation program, while group B (non derotation group, without vertebral derotation, NdRG) received posterior correction and the same rehabilitation program.
Pulmonary function tests (forced expiratory volume (FEV1) and maximum voluntary ventilation (MVV)) were measured by using a spirometer (Chest Graph Hi-101) while the patients were positioned in a sitting position according to the American Thoracic Society. Each participant has been instructed to inspire deeply, and then expire forcefully and rapidly for FEV1. This manoeuvre was repeated 10 consequent times to detect the MVV [8].
Measurements of the Cobb angles were done by using X-ray; which was taken from anteroposterior and lateral views of the spine from a standing position (stress X-ray) [9].
A rotational ruler was used to measure the degree of vertebral rotation. The ruler was placed on the anteroposterior X-ray. The angle between the two lines was measured as the straight line that passed through the outer border of the vertebra and the diagonal line that passed through the middle of the pedicle [10].
Measurements of the chest expansion were done using a palpmeter. With the participant in a standing position, the two ends of the palpmeter were placed horizontally around the chest, at the xiphoid process level. Two palpmeter limbs moved laterally during inspiration and returned to their original position during expiration, allowing measurements of the differences from a scale connected to its limbs.
Evaluation of the measuring variables was carried out pre-operative, immediately post-operative, and three months after the operation. Both groups started the program on the first day after the operation by being taught the perfect breathing approach and adapted daily living activities. Post-operatively, participants were treated with a pulmonary rehabilitation protocol, 3 sessions per week for 3 months.
For training and education for normal breathing, the program started immediately after the operation using an incentive spirometer. Each patient was asked to inspire via a mouthpiece and then detect the gained volume. They were instructed to inspire and then hold the plastic detector at a specific point, before continuing training, with ten repetitions per set.
To train the elastic recoil of the lungs and regain good distribution of air, three different forms of segmental breathing exercises, each with ten repetitions (apical-costal and posterior) and applied in a sitting position. To increase the oxygen saturation and improve the physical work capacity, a treadmill was used for training after 10 days post-operative by asking the patient to run at a speed equal to 1.5 km per hour with a zero inclination angle and begin the exercise gradually for 30 min/session for three months.
Statistical analysis data were assessed for the assumption of normality and variance homogeneity. Normality testing via Shapiro–Wilk revealed normal data distributed (p > 0.05) after outliers were removed, and the outliers were addressed using box and whiskers plots. As well, variance homogeneity via Levene’s test recorded no significant differences (p > 0.05). Thus, normal data distribution was ensured and parametric analysis was conducted.
Statistical SPSS Package version 25 for Windows (SPSS, inc., Chicago, iL) was used. Mean and standard deviation were manipulated for expressing data on patient clinical general characteristics, Cobb angle, angle of rotation, chest expansion, and pulmonary function (FEV1 and MVV) variables. T-tests ‘independent’ were performed to compare dRG versus NdRG groups for the general characteristic variables. A chi-square test was performed to compare dRG versus NdRG for gender variables. A mixed MANoVA test was performed to compare both groups ‘between and within’ for Cobb angle, angle of rotation, chest expansion, and pulmonary function (FEV1 and MVV) variables. Bonferroni correction test (post-hoc test) was performed to compare pairwise groups ‘between and within’, in cases of a significant MANoVA test. All statistical analyses were significant at probability (p 0.05).
Results
The raw data of both Cobb and rotation angles, chest expansion, and pulmonary functions (FEV1 and MVV) were analysed to detect baseline and 3-month post-treatment means and standard deviations. MANoVA-test has been applied to assess the treatment effect.
Patient clinical general characteristics
This study includes a total of 56 participants of both sexes diagnosed with AiS, with participants allocated into two equal groups. Non-significant differences (p > 0.05) in patient’s age (p = 0.507), height (p = 0.361), weight (p = 0.694), BMi (p = 0.986), and sex (p = 0.487) were confirmed between the groups (Table 1).
Table 1
General participants’ clinical features in both groups
Curve correction (mechanical parameters)
Cobb angle
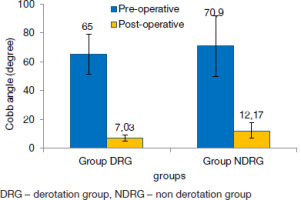
Comparing Cobb angle mean values indicated non-significant differences (p > 0.270; p > 0.05) between both groups. A significant reduction in the Cobb angle was observed within both groups either at baseline or post-operative, while a remarkable reduction was revealed in group A (p = 0.0001; p < 0.05) when compared to the post-operative mean values of both groups. Post-operative mean values were 7.03 ± 2.06° for group A and 12.17 ± 5.32° for group B (Table 2 and Figure 1). This represents a percentage of improvement in Cobb angles of 89.18% and 82.83% for groups A and B, respectively (Table 3).
Table 2
Within and between group comparison for ventilatory functions and chest circumference
Table 3
Mean difference and change percentage for ventilatory functions and chest circumference within each group
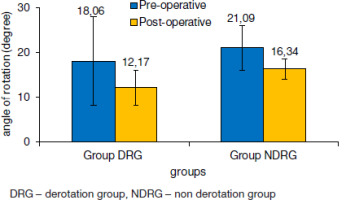
The angle of rotation
Comparing the mean values of the angle of rotation indicated non-significant differences (p = 0.517; v > 0.05) between both groups at the baseline of the study. A significant reduction in the angle of rotation was observed in both groups either at baseline or post-operative, while a remarkable reduction was revealed in group A (p = 0.0001; p < 0.05) when compared to post-operative mean values of both groups. The post-treatment mean values were 12.17 ± 3.93° for group A and 16.34 ± 2.32° for group B (Table 2 and Figure 2). This represents a percentage of improvement in the angle of rotation of 32.61% and 22.52% for groups A and B, respectively (Table 3).
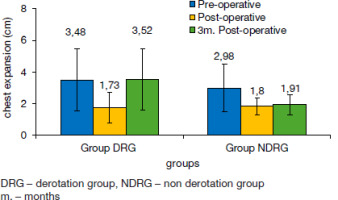
Chest expansion
Comparing the mean values of chest expansion indicated non-significant differences between both groups at baseline. Significant reduction in chest expansion was observed in both groups either at baseline or post-operative, while a remarkable reduction was revealed in group A (p = 0.0001; p < 0.05) when compared to group B post-operative mean values (p = 0.029; p < 0.05). Mean values were 1.73 ± 0.96 cm for group A and 1.8 ± 0.51 cm for group B (Table 2 and Figure 3). This represents a percentage reduction of 50.29% and 39.60% for groups A and B, respectively (Table 3). At three months post-operative, both groups showed obvious improvements (p = 0.001; p < 0.05) equal to 3.52 ± 1.97 cm and 1.91 ± 0.60 cm for groups A and B, respectively (Table 2 and Figure 3).
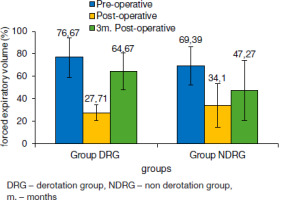
Ventilatory functions (physiological parameters)
The mean values of FEV1 at pre-operative were 76.67 ± 17.79% and 69.39 ± 16.91% for groups A and B, respectively. The mean values of FEV1 immediately post-operatively were 27.71 ± 7.05% for group A and 34.1 ± 19.25% for group B, with a significant reduction in both groups, which was highly significant for group A. At three months post-operative, both groups showed obvious improvements (p = 0.0001; p < 0.05) with mean values equal to 64.67 ± 16.44% and 47.27 ± 26.69% for groups A and B, respectively (Table 2 and Figure 4). This represents a percentage reduction of 63.86% and 50.86% for groups A and B, respectively (Table 3).
Figure 4
Mean values of forced expiratory volume (FEV1, %) at baseline, post-operative, and 3 months later for groups A and B dRG – derotation group, NdRG – non derotation group m. – months
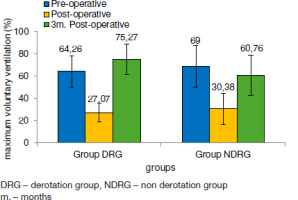
Mean MVV values at pre-operative were 64.26 ± 14.06% and 69.00 ± 18.84% for groups A and B, respectively. Mean MVV values immediately post-operatively were 27.07 ± 8.25% for group A and 30.38 ± 14.39% for group B, with a significant reduction within both groups, with a remarkable reduction in group A. At three months post-operative, both groups showed obvious improvements (p = 0.001; p < 0.05) with mean values equal to 75.27 ± 13.57% and 60.76 ± 18.31% for groups A and B, respectively (Table 2 and Figure 5). This represents a percentage reduction of 57.87% and 55.97% for groups A and B, respectively (Table 3).
Discussion
This study was conducted to evaluate vertebral derotation effects on pulmonary function and chest expansion after surgical correction of AiS.
The influence of the vertebral derotation technique on pulmonary function, as a physiological parameter, or on curve correction and chest expansion, as a mechanical parameter, has been inadequately examined.
The study results correspond to the findings of [11, 12], who declared that there was a 20%–40% decrease in chest expansion and respiratory system compliance. These outcomes began immediately following surgery.
Turner et al. [13] revealed a significant decrease in FVC following dorsal fusion of the spine through thoracoplasty, even in minor interventions, unless a remarkable FEV1 improvement following dorsal fusion of the spine was seen. Furthermore, dorsal fusion of the spine alone and dorsal fusion of the spine through thoracoplasty had no influences on both FEV1 and FVC among AiS participants who had mild curvatures on follow-up for a couple of years. Therefore, thoracoplasty may be useful for those who have cardiopulmonary disease.
Scoliosis patients had reduced respiratory system compliance, particularly diminished thoracic wall compliance, which is a significant factor regarding restricted volumes and has a tight link with scoliosis severity and a decrease in FVC [8].
Reduced volumes of the lung measured by a fall in the total capacity of the lung have been linked to restrictive lung disease, which is thought to be more common in people with scoliosis. The decrease in total lung capacity and the corresponding fall in FEV1 and FVC are negatively related to scoliotic-measured Cobb angles [14].
A positive correlation between scoliosis and restricted pulmonary function attracted more attention among AiS than among idiopathic adults. Because respiratory functional development in young patients is still in the growth period, respiratory function following corrective surgery may differ from that in adult patients. Associated growth related to pulmonary function was typically fast and nonlinear throughout the adolescence era, where it peaks at fourteen for males and twelve for females [15].
The participant’s quality of life is greatly improved by surgical correction of spinal abnormalities, and can resume normal activities with just mild impairment. The operations are feasible and safe, correcting deformities by a mean of 59% and enhancing respiratory function by a mean of 50%. These factors lead to statistically and clinically substantial increases in quality-of-life outcome ratings and decreases in back pain [16].
No evidence recommends surgical intervention to enhance the scoliotic population’s quality of life. Thus, there is an actual need for further clinical randomised trials that might address the suspected benefits of surgical approaches [17].
The present study’s results are in line with the findings of [12], who reported that scoliotic patients remained at risk for post-operative problems up to one week after surgery and a delayed regain of pre-operative pulmonary capabilities up to a couple of months. Post-operative deterioration of lung capacities should be included by evaluating the risk-benefit ratio pre-operatively.
Furthermore, in agreement with [18], who compared initial thoracic compliance, including lateral bending radiographs, revealed that restricted participants who had a less dorsal curvature restriction nearby (46%), were substantially superior to controls by 35% (p = 0.03). The remaining pre-operative variables for both cohorts were comparable.
Kempen et al. [19] explored the connection between a patient’s pulmonary function and the degree to which their scoliosis has progressed in individuals less than 21 years old. The thoracic Cobb angle has an adverse relationship with VC, FVC, and FEV1, as well as TLC either predicted or absolute. Additionally, a strong association was found between the anticipated FRC and the sharpness of the curve.
Both outcome measures involving MEP and MiP were assessed initially, after one and six months, which revealed remarkable improvement post-treatment, indicating that surgical scoliosis correction for such individuals enhances good influence on the strength of the respiratory musculature [4]. in patients with thoracic-dominant scoliosis, both doppler for tissue E’/A and mitral E/A ratios had a strong negative correlation to the angle of Cobb. dorsal deformity of the cage might restrict heart diastolic motion as seen by PFT’s limited pulmonary capacities, also impaired venous return has a negative impact on the earlier atrioventricular flow phase and contracting atrium [5].
Curve correction via vertebral derotation leads to a realignment of bone components, resulting in the elimination of the hump as well as the re-establishment of average normalisation of muscle position and functional activity, and ligaments will be in the elastic zone rather than the plastic region, as in an unfused vertebra. This mechanical adjustment affects pulmonary functioning [20].
The surgically treated individuals had significantly decreased thoracic range of motion than those who received brace only and control groups. Thorax cage volume plus respiratory movements while maximal respiration was considerably lower in scoliotic individuals than in controls, with no significant differences between treatment groups. TLC, FVC, and FEV1 showed that participants who were treated with a brace had improved lung function in favour of others. When compared to reference values, only surgically treated individuals had significantly poorer respiratory muscle strength. A multivariate analysis found that the participant’s sex, bracing approach, and smoking were the primary predictors explaining the TLC proportion anticipated [9].
No obvious alterations in traditional spirometry (FEV1 and FVC) in 37 female scoliotic children where the angle of curvature means was 32.8°. However, the researchers raised attention to somewhat lower exercise tolerance in scoliosis-affected girls. These modifications were related to the curvature angle [21].
Current study results come in agreement with [22] who stated that the pulmonary function test increases significantly in the third month after surgery, whereas there is no improvement after one year.
Also, similar findings have been demonstrated by [23], who neglected any valuable improvement according to spirometry measures after surgical intervention for those suffering from mild to moderate AiS.
Smaller body mass index and bigger thoracic transverse and anteroposterior diameters were consistent characteristics of patients with clinically significant PFT impairment. Clinical impairment was associated with greater thoracic height, angle of scoliosis, and its extent on spinal vertebrae. The angle of scoliosis and vertebrae number affected, as well as dorsal diameter in the sagittal plane, were considerably negatively correlated with PFTs, while thorax height was significantly positively correlated. PFTs were unrelated to height at the T1–12 level. The PFTs of individuals with rib anomalies, especially those with fused ribs, were considerably lower than those of patients without rib anomalies [24].
Lin et al. [25] confirmed that the thoracic cage degree of deformity correlated with reduced pulmonary static function. Additionally, asymmetry and rib cage deformation were also linked to irregular breathing patterns and decreased exercise capacity. despite the lack of sufficient evidence of any therapeutic benefits on lung function for exercise training of AiS, the authors anticipate that whole lung capacity, also laboratory parameters might renormalise with extended rehabilitation respiratory training. Furthermore, many clinical trials discovered that satisfied surgical AiS patients regarding their pain, daily and functional activity, overall mentality and appearance, and contentment [26].
Limitations
Our study has certain drawbacks. The authors admit that they did not conduct a thorough examination of their patient’s lung function. in the subsequent stage of the investigation, they plan to conduct more in-depth spirometry and body plethysmography diagnostics to acquire a more comprehensive understanding of the respiratory system.
Conclusions
In addition to its beneficial effects on curve correction and angle of rotation, the vertebral derotation technique has an adverse impact on physiological parameters (pulmonary functions) as well as mechanical parameters (chest expansion) immediately post-operatively. However, a beneficial effect was detected following three months of a pulmonary rehabilitation program in all parameters.