Introduction
Generalised anxiety disorder (GAD) is defined as tension, trepidation, fear, or apprehension arising in response to situations or events that are typically regarded as normal, are difficult for the person to manage, and persist for at least six months [1]. Factors contributing to GAD development are biological (diet, sickness, and neurotransmitter imbalance), psychological (personality characteristics, self-confidence, cognitive discord, unfavourable feelings, interpersonal and intrapersonal conflict, crisis of development), and social (negative life events, stress at work, lack of social skills, lack of social support, altering values, conflict of societal norms, and natural disasters) [2].
Musculoskeletal disorders (MSDs) are a serious global health issue [3], with 11 to 50% of the general population suffering from chronic disease [4]. The term “work-related musculoskeletal disorders” (WMSDs) refer to conditions brought on by or exacerbated by the workplace, including complaints of pain, tingling, swelling, or discomfort in different regions, including the neck, shoulder, back, elbow, wrist, hip, knee, or multiple other joints, within the previous 12 months [5]. WMSDs are caused by applied forces, repetition, vibrations, awkward postures, moving objects, lifting patients, bending, twisting, and abrupt movements [6].
Doctors save lives (protectors), but when they are under physical or psychological strain or some other problem that interferes with their quality of life, their performance suffers, which could have a negative outcome on patients [7]. A population of Asian nurses had an annual MSD prevalence rang ing between 40 and 95% in at least one body part and/or region [8]. Furthermore, 90% of physiotherapists have WMSDs, with 50% of cases appearing during the first five years of employment due to uncomfortable positioning, inadequate lifting technique, and poor posture [9].
Since anxiety has a detrimental effect on professional development and reduces patient care quality, it demands more consideration in the medical field [10]. Resident doctors in accident and emergency departments had higher rates of anxiety, with severity levels ranging from moderate to severe [11, 12]. Compared to other diseases, anxiety is the primary cause of absenteeism due to illness. in addition, people spend a large portion of their life at work, which affects their health and risk of disease.
Msds contribute to the burden of disability and are closely linked to the global ageing process. The current research accounts for occupational risk factors in addition to personal /behavioural risk factors [13]. Many studies have researched the relationship between anxiety and MSDs, and the current study will add to this important topic. The findings will serve the healthcare community by providing information about the association between these two critical factors and the extent to which they affect each other.
Subjects and methods
This analytical cross-sectional study used a non-probability convenient sampling technique to enrol the participants. After receiving ethical approval (ER # 704/ ERC/CMH/LMC) and institutional permission, informed consent was obtained from the participants before data collection. The targeted population was medical professionals from different hospitals in Lahore. inclusion criteria were aged 20-40 years, male or female gender, medical professionals (including physicians, surgeons, dentists, physical therapists, pharmacists, radiologists, and nurses), a history of musculoskeletal problems, anxiety symptoms for more than two weeks, and a willingness to participate. Exclusion criteria were traumatic events, such as road traffic accidents, fractures, ligament injuries, and nerve injuries, a psychological disease diagnosis other than GAD, pregnancy (2nd and 3rd trimester), and less than one year of professional experience. Data analysis employed SPSS version 22.0, with frequencies and percentages calculated for quantitative and qualitative variables and results expressed using figures (bar charts and pie charts). Chi-squared (X2) and Cramer’s rule assessed the association between GAD and WMSDs. The sample size was calculated using the formula:
The study sample size was 260 [14].
Results
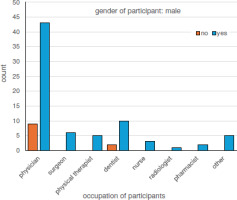
Figure 1 shows the occupation of male participants and the prevalence of MSDs, which were most prevalent among physicians and least among radiologists. Table 1 shows the weak positive association between MSDs and GAD among the 260 participants (p = 0.01, Cramer’s V = 0.22).
Table 1
Cross tabulation of generalised anxiety disorder and musculoskeletal disorder prevalence (n = 260)
Table 2 shows the association between MSDs and GAD, which was not significant among the 86 male participants. However, the relationship was statistically significant among the 174 female participants (p = 0.043, X2 = 8.166).
Table 2
Cross tabulation of generalised anxiety disorder and musculoskeletal disorder prevalence among genders
Discussion
Medical professionals were shown to experience significant musculoskeletal pain incidence, which resulted in depression and anxiety. A severe workload, fear of contracting an infectious disease, stress, and other factors might make healthcare personnel less focused and negatively impact their performance. Therefore, assessing preventative practices and the mental health and musculoskeletal systems of healthcare personnel is crucial [14]. This study aimed to identify the association between GAD and WMSDs among medical professionals and determine whether all were affected in the same way or whether others were more vulnerable due to their field.
Gad is one of the most prevalent anxiety disorders and can cause significant issues, such as extreme mental distress and depression. To rule out this problem and improve daily living, early detection is essential. in previous articles [15], the GAD-7 scale evaluated GAD, and the Nordic musculoskeletal questionnaire detected MSDs [16]. Healthcare workers had a high proportion of work-related musculoskeletal discomfort, with the neck, lower back, and upper back areas being most affected, and a mean GAD score of 6.36 ± 5.42.
Alharthy et al. [11] found that 52% of emergency medical professionals experienced anxiety to varying degrees. indeed, 48% reported being in good health after completing the GAD-7, and 23.7% reported mild anxiety symptoms. Meanwhile, 20.7% with a moderate score were likely to receive an anxiety diagnosis, and 7.4% of participants with significant anxiety were more likely to develop an anxiety disorder [11]. A correlation between gender and anxiety was also discovered, with anxiety scores higher in women than men and females more likely to develop GAD, similar to the current study.
Most male and female participants fell into the minimal anxiety category, and it appears that lower back (27%) and neck (26%) pain prevented normal work the most in the last 12 months. Arca et al. [14] concluded that neck and lower back pain affected everyday activities the most (42%), with pain and incapacity to work influencing diverse anatomical regions over a range of occupational categories and time intervals [17]. Other researchers showed that 68.4% of the general population with neck pain were dealing with stress, while 55.7% were diagnosed with depression [18].
We found that female medical professionals with musculoskeletal problems were more prone to GAD than male medical professionals, which is in line with other studies showing that women experience depression more than males [19]. A plausible explanation for this finding is that the longer reproductive life of females compared to males contributes to their increased risk of depression [20].
Limitations
The non-probability convenient sampling technique used increased the risk of bias, while the use of self-reported data introduced the potential for recall bias. Furthermore, limited data was collected from senior medical professionals and surgeons with 10-15 years or more experience, with most responses collected from professionals with 1 to 2 years of experience.