Introduction
Mastectomy is a surgical method that involves removing the diseased part of a woman’s breast, along with a surrounding area of healthy tissue, until no cancer cells are detected at the boundaries of the excised tissue. A simple (or total) mastectomy involves the full removal of the breast tissue [1].
Lymphoedema is characterised by enlargement of the breast’s tissues due to the growth of fluid containing proteins in the gaps between cells. The symptoms manifest in the arm, hand, and trunk, resulting in limb pain, heaviness, and impaired sensations [2]. The condition is a result of a reduced ability of the lymphatic tissues to transfer fluids and/or an increase in the amount of fluids that the lymphatic system needs to transport. It also stems from the buildup of fluid in the extracellular spaces that is high in proteins [3].
The presence of functional, aesthetic, and psychological issues had a negative effect on the functional activities and quality of life (QOL) of individuals diagnosed with lymphoedema. It also makes patients more susceptible to acquiring infections, reduces their functional capacity and range of motion (ROM), and increases the risk of developing malignant lymphangiosarcoma [4].
Upper-extremity lymphoedema is a prevalent physical consequence that often occurs following breast cancer therapy. It is defined by chronic swelling of the tissues in the affected limb, caused by an abnormal build-up of lymph fluid [5]. There is currently no cure; however, therapies can alleviate symptoms and potentially prevent or delay the disease’s course [6].
Physical therapy is crucial for treating lymphoedema characterised by swelling in the upper limbs. Various therapies, such as-CDT, ultrasound, cryotherapy, laser therapy, electrotherapy, resistance training, along with Kinesio taping, have been suggested to reduce swelling in addition to limiting the consequences associated with lymphoedema [7, 8].
Despite the extensive evidence supporting the effectiveness of CDT-in treating lymphoedema [9–11] according to reports, a more comprehensive and effective therapy can be achieved through the use of combination approaches [6]. It is crucial to treat lymphoedema among-breast cancer patients as it can improve their QOL [12].
Applying active resistance exercise with CDT-to patients suffering breast cancer-related lymphedoema does not result in increased swelling. Furthermore, it considerably reduces the volume of the upper arm and helps improve the QOL [2].
Alternative and physical therapists now have KT as an option for lymphatic drainage. The KT material was created to accommodate a longitudinal stretch of 30–40%. This product is made using acrylic heat-sensitive adhesive and 100% cotton fibres. KT’s physiological benefits include alleviating pain or aberrant feeling, facilitating muscular mobility, relieving lymphatic fluid congestion and subcutaneous haemorrhages, and realigning joints that are out of alignment [13].
Applying KT results in the formation of convolutions in the taped area, which effectively increases the gap between the muscles and the skin. When the skin is raised, it enhances the circulation of blood and lymphatic fluid [14].
Cryotherapy is a new therapy modality used for many purposes, including pain, inflammation, and oedema. Skin cooling initially leads to local vasoconstriction [15] and decreases the normal post-ischemic hyperaemic response caused by tissue indentation loading [16]. Skin cooling also leads to systematic vasoconstriction [17].
The local vasoconstriction also leads to decreased capillary fluid filtration and increased post-capillary fluid reabsorption. All this results in a decreased interstitial fluid volume. Lymphoedema is also often associated with inflammation and fibrosis, so cryotherapy, which produces cooling to a depth of about 2–4 cm, might be having a positive effect on this condition [18].
To our knowledge, there have been few studies that look at the effect of different physical therapy modalities such as CDT, KT and cryotherapy in post-mastectomy patients, but none that look at the effect and comparison between them to detect the best in treating lymphatic patients after mastectomy. It was hypothesised that there is no effect of using cryotherapy, CDT and KT in post-mastectomy patients. So, this study aimed to evaluate the effect of CDT, cryotherapy and KT in patients with post-mastectomy lymphoedema.
Subjects and methods
Design of the current study
The study was randomised and single-blinded. All patients provided their informed consent to participate, and the study was conducted from March through December 2023.
Sample size calculation
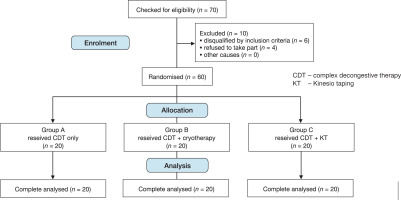
We used the G*POWER statistics program (version 3.1.9.2; Franz Faul, Universitat Kiel, Germany) to conduct an F-test MANOVA with both within-and between-interaction effects. It was necessary to establish a sample size of 60 patients, with 20 participants per group, taking into account a = 0.05, power = 76%, and effect size = 0.71.
Randomisation
As shown in the flowchart in Figure 1, 70 patients met the inclusion criteria for the study, but 10 of them dropped out because they lived too far away. It was used to randomly assign the remaining sixty patients with a 1:1:1 allocation ratio. Concealed allocation was done using sealed, sequentially numbered opaque envelopes. It is challenging to divide samples into three equal groups with the same numbers in this randomised program due to the presence of multiple stratified variables [19]. The randomisation was carried out by a blinded researcher who was not involved in recruiting, data collection or treatment.
Participants
Sixty women with post-mastectomy lymphoedema were referred by their surgeon, who confirmed their diagnosis as post-mastectomy. They were recruited from Baheya Hospital and the Cancer National Institute, Giza, Egypt. The studies were carried out at the outpatient clinics of the Faculty of Physical Therapy, Modern University for Technology and Information in Cairo, Egypt.
The criteria for inclusion were as follows: (a) patients aged 40 to 60 [14], (b) Stage 2–3 lymphoedema [3], (c) a difference of over 2cm at the circumference measurement, (d) unilateral arm lymphoedema post-mastectomy, and (e) having completed chemotherapy and radiotherapy. Patients with (i) skin infection, (ii) current ischemia, (iii) Systemic oedema resulting from compromised cardiac, renal, and hepatic function, (iv) present metastases, or v) venous thrombosis were excluded.
The participating patients were divided into three groups of equal size. Each participant in the three groups was administered an identical CDT program: group A was administered CDT only, Group B was administered CDT and cryotherapy, and group C was administered CDT and KT. The treatment program was applied 3 sessions/week for 12 weeks.
Measurements used
Arm girth measurement (cm) measured by circumferential measurements
This is a valid and reliable method. Throughout the study, the protocol was implemented, with measurements taken on both limbs at the axilla, halfway between the axilla and the cubital fossa, at the cubital fossa, halfway between the cubital fossa and the wrist. The participants were asked to sit with their arms resting on a table, their shoulders slightly bent forward, and their elbows bent at 45 degrees. The measurement site at the wrist and the other measurement sites were marked on the skin using a pen at predetermined distances from the wrist [20].
Pain severity measured by VAS
This was typically performed on a line that is 10 cm (100 mm) in length, with the ends typically labelled with verbal pain anchors (e.g., “pain as bad as it could be” and “no pain”). Patients are requested to identify the point on the line from 0 to 10 cm, which is marked in 1-cm increments. 0 cm denotes no pain, while ten cm denotes the maximum pain presented. It is also an interval scale, so it can be employed in clinical practice as an outcome measurement tool for pain measurement [21]. VAS was demonstrated to be valid and reliable in the majority of the investigations [22].
QOL measured by SF-36
This is a generally accepted and commonly used approach for evaluating the QOL of patients. The reliability and validity of the SF-36 have been assessed in numerous specialised populations globally [23]. The assessment includes a multi-item scale that evaluates eight health concepts, with each concept consisting of 2 to 10 questions. These concepts are: physical functioning (PF), role limitations because of physical problems (RP), bodily pain (BP), general health perception (GH), vitality (VT), social functioning (SF), role limitations owing to emotional problems (RE), as well as mental health (MH). Lower scores indicate restrictions in QOL [3].
Range of motion (ROM) measured by UG
The device, commonly utilised in China, is regularly employed by physical therapists to measure the shoulder ROM. This device is preferred due to its simplicity, portability, noninvasive nature, and affordability [24]. This UG is commonly utilised in several studies on the validity of using alternative devices for ROM measurement due to its high inter- and intra-rater reliability for evaluating ROM in the upper extremities [25] (Table 1).
Intervention
Complex decongestive therapy (CDT)
As shown in Table 2, CDT was applied in every treatment session, which included manual lymphatic drainage (MLD) [26], compression bandage [27], exercises to augment lymphatic drainage [28] and skin care [29].
Cryotherapy
A cryo-air machine (CRYO MINI, Professional Cooled Air Therapy System, USA), which utilises cryo-air cold air therapy technology, is a mature and safe-to-use system that cools the air to –32°C. The application steps were: (1) before undergoing cryotherapy, hydrate the skin with an oil or cream, (2) initialise the mini cryo-air equipment at level 6, (3) it was applied 5 min; this orientation corresponds to that lymphatic fluid flow in the direction from distal-to-proximal at every point on the hand, wrist, forearm, and arm [30].
Kinesio taping (KT)
This represents a novel alternative form of physiotherapy. It was introduced by Dr Kenso Kase in 1973. K-tape was intended to accommodate a longitudinal stretching of 30–40% [31]. The method was performed while the patient was seated, with the upper limb flexed at a 90° angle and the elbow joint extended. The K-tape was specifically placed on the upper limb in a double fan shape, encompassing the arm and forearm. KT is done without applying any tension to the skin, which had already been stretched to its utmost capacity, resulting in the formation of convolutions. A lymph physiotherapist also carefully ensured that it was consistently maintained for a duration of 24 hours every day, and thereafter replaced every seven days [32].
Table 1
Range of motion measurement of shoulder flexion, extension, abduction and external rotation
Table 2
Complex decongestive therapy program
Statistical analysis
The statistical analyses were computed using the Statistical Package for the Social Sciences (SPSS) version 20. The data in the current investigation were reported as the mean values and standard deviations. The Shapiro–Wilk test was employed to confirm that the data adhered to a normal distribution. In order to assess the presence of homogeneity in the variations among different groups, Levene’s test was performed. The measured outcomes were compared across groups using unpaired t-tests, and within each group, the study variables pre- and post-treatment were compared using paired t-tests. To ensure that there was no type I error, we used two-way mixed-model multivariate analyses of variance (MANOVA) to compare the groups’ mean change scores for all outcomes, and we used Bonferroni-adjusted p-values for each outcome measure. The differences among the three groups were examined via ANOVA followed by a least-squares difference (LSD) post hoc test. The alpha threshold for all tests in this study was established as 0.05.
Results
Demographic data
When comparing the age-related mean values of groups A, B, and C, we found no statistically significant differences (p > 0.05) (Table 3).
Variables of measurement
(1) Pre-treatment comparison between groups A, B and C. The comparison between the pre-treatment mean ± SD values in all measurable variables was revealed among the 3 groups (p > 0.05) (Table 4).
(2) Comparison of pre- and post-treatment within groups A, B and C. Between the pre- and post-treatment comparison mean ± SD values of all measurable variables were revealed among the 3 groups (p < 0.05) (Table 4).
Table 3
Age comparison between groups (A, B and C)
| Group A (mean ± SD) | Group B (mean ± SD) | Group C (mean ± SD) | f-value | p-value | |
|---|---|---|---|---|---|
| Age (years) | 50.35 ± 5.55 | 49.35 ± 6.66 | 48.55 ± 4.75 | 0.17 | 0.841NS |
Table 4
Comparison of arm girth measurements, VAS, SF-36 and shoulder ROM for the three groups (A, B and C)
(3) Comparison of post-treatment between groups A, B and C. The comparison among the post-treatment mean ± SD values of all measurable variables was revealed within the 3 groups (p < 0.05) (Table 4).
(4) Comparison of post-treatment between groups A and B, groups A and C, and groups B and C. When comparing the post-treatment mean ± SD values among groups A and B, A and C, and B and C, all measurable variables were statistically significant between the two groups (p < 0.05) (Table 5).
Discussion
The effect of CDT, cryotherapy, and KT on patients suffering from lymphoedema following a mastectomy was examined. There were substantial differences across all measurable variables prior to and following treatment in the three groups. Meanwhile, the significant difference is presented post-treatment, favouring the cryotherapy group in comparison to the KT group and the cryotherapy and KT groups.
The pre-and post-treatment comparison results of group A are in agreement with those of Mobarakeh et al. [33], who demonstrated the effects of CDT in the treatment of lymphoedema that comes with breast cancer. Currently, CDT therapy is the primary treatment option for lymphoedema. The therapy’s effect is predominantly affected by factors such as experience, specialisation, patient activities, and compliance [6].
In another study that agrees with our findings of group A, Corum et al. [34] discovered that the combination of CDT and resistance training proved to be successful in decreasing circumference, volume, pain, and functional impairment, while also enhancing grip strength and QOL.
Table 5
Comparison post-treatment of arm girth measurements, VAS, SF-36 and shoulder ROM between groups A and B, groups A and C, and groups B and C
Ozcan et al. [10] conducted a study to investigate the impact of CDT on upper extremity functioning, pain intensity, and QOL. It was shown that the VAS scores decreased considerably following CDT. In addition, Mobarakeh et al. [33] observed notable reductions in VAS severity, aiming to evaluate the efficacy of CDT and determine the minimum session sets required to achieve significant pain reduction among patients suffering breast cancer-related lymphoedema.
Park et al. [35] demonstrated that there were significant reductions in limb circumference measurements in their group A following CDT, indicating substantial differences compared to other groups. Nevertheless, substantial enhancements were observed. The improvement in the shoulder function was accomplished by increasing the ROM values and substantially decreasing the VAS scores.
In group A, patients who received CDT experienced a substantial decrease in oedema, along with an improvement in functionality. This improvement in functionality may be attributed in reducing the oedema presented on the limb, which aligns with the results of Didem et al. [36], who revealed that CDT has positive effects on the volume of extremities, pain, and QOL among patients who develop breast cancer (lymphoedema). In addition, Kim et al. [37] documented a decrease in the volume of lymphoedema by the use of CDT.
The results of our study conducted on Group B indicate that cryotherapy is an adjunctive technique that has a substantial beneficial impact on pain intensity. This agrees with a prior study conducted by Askary and Elshazly [30], which showed a substantial reduction in the thickness and circumference of the wrist, below the elbow, and above the elbow in the intervention group (cryotherapy) in comparison to the control group (conventional physical therapy).
Gutiérrez-Carmona and Alvarez-Marín [38] corroborated the results of group B by stating that pain experienced during cryoanalgesia and topical anaesthesia is identical. They proposed that cryoanalgesia is a viable treatment for patients involving allergies to anaesthetics. The study applied by Mayrovitz and Yzer [39] found that skin cooling of about 24% to 28% of the upper limb softens lymphoedematous and fibrotic tissue. This softening of the tissue leads to decreased pressure in the underlying nerve ending and decreased input to the sensory nerves, which interrupts the pain cycle.
Silva et al. [40] proposed that cryotherapy exerts analgesic effects through cold-induced vasoconstriction that reduces blood flow to tissues, thereby decreasing the release of inflammatory mediators. It also helps local anaesthetics accumulate in the target tissue.
The findings from secondary studies support the findings of Group C, as demonstrated by Tsai et al. [41]. According to their study, applying KT techniques induces physiological effects such as reducing pain or abnormal sensation, facilitating muscle movement, alleviating congestion of lymphatic fluid and haemorrhages in the skin, and correcting joint malalignment.
The findings of Lipińska et al. [42] verify the outcomes of group C. Their study followed women with breast cancer lymphoedema who got KT therapy for 20 days in the upper limb. The efficacy of this KT therapy after mastectomy was demonstrated by a 24% reduction in oedema, a 20% increase in ROM, and normalisation of muscular tension.
The results of group B, which showed greater effectiveness compared to groups A and C, align with the findings of Silva et al. [40], who observed that cryotherapy possesses anti-inflammatory and analgesic properties. Nadler et al. [43] reported that cryotherapy decreases the nerve fibre conduction velocity by disrupting the synchronised transport of pain fibres. There is a suggestion that using a cold solution inside the eye during phacoemulsification surgery can help avoid the continual transmission of mechanical pain signals.
The post-treatment outcomes for group C showed an improvement that was statistically significant compared to those of group A, which is consistent with the outcomes of Pekyavaç et al. [3]. They also discovered that combining CDT and KT was more successful in reducing volume and improving QOL. Kase et al. [13] found that combining CDT with KT application extends the duration of the lymphoedema treatment’s effectiveness. One possible explanation for this is that the KT lymphatic correction method stimulates lymphatic circulation by raising the top layer of skin and increasing the volume of the layer underneath it, which contains lymphatic capillaries. This increases the pressure on the fluid surrounding the cells.
These findings contradict the results of Hemmati et al. [6], who found that there were no substantial differences in limb circumference changes across the research groups when cryotherapy was used. Our study’s results are also inconsistent with the findings of Fong et al. [44], who observed a decrease in strength in flexion, extension, abduction, in addition to internal and external rotation movements following lymphatic surgery. However, they did not find any substantial differences in the ROM-assessments.
Limitations
This study has some limitations related to changes in the patients’ lifestyle habits and educational levels, differences in motivation between all patients – some patients did not complete the treatment protocol for various reasons and were excluded from the study – possible conflicts with knowledge gained from course work, and a lack of knowledge of whether the skills will transfer to a clinical environment.