Introduction
Peripheral nerve lesions (PNLs) are a group of distinct disorders that can be caused by car accidents, falls, work accidents, household accidents, and penetrating trauma. Seddon and Sunderland made the first classification of nerve injuries, which is still used today and is still correct. The three main types of nerve injuries are neuropraxia, axonotmesis, and neurotmesis [1].
Pnls can occur symmetrically throughout the body, such as polyneuropathy in single nerves or mononeuropathy in multiple. Polyneuropathy usually occurs secondary to diseases such as leprosy, human immunodeficiency virus (HIV) infection, Guillain-Barre syndrome, rheumatoid arthritis, chemotherapy, and diabetes mellitus, while mononeuropathy affects a discrete nerve and results in local syndromes such as carpal tunnel syndrome, cubital tunnel syndrome, and tarsal tunnel syndrome [2, 3]. PNL diagnostic procedures typically require electromyography (EMG), a nerve conduction study (NCS), or specific laboratory investigations to confirm the diagnosis [4].
Low-level laser therapy (LLLT) reportedly activates nerve cells, improves nerve cell energy use, and accelerates nerve sprouting processes. Researchers found that using laser therapy to treat damaged nerves had instant protective effects, including enhanced nerve function, reduced scar tissue at injury sites, less degeneration of the corresponding spinal cord motor neurons, and substantially more axonal growth and myelinisation. In addition, applying laser therapy directly to the spinal cord improved the function of damaged peripheral nerves [5].
Lllt has been shown to cause immediate nociceptor blockade (pain relief) and accelerated self-healing. In addition, LLLT can enhance fibroblast proliferation and neovas- cularisation, promote angiogenesis, and increase collagen synthesis to aid acute and chronic wound healing [6].
Evidence-based practice entails the deliberate use of various information sources and the best available evidence, such as published research, along with clinical judgement and patient values and preferences [7] (as determined by a systematic search for and critical appraisal of the evidence most related to answering a clinical question) [8, 9].
Laser therapy may have effects on peripheral nerve regeneration, though more studies are needed to support this. Therefore, this systematic review investigated the effects of LLLT on PNL regeneration. if the study demonstrates that LLLT is as safe as conventional physiotherapy for sensory nerve regeneration and pain intensity treatment, LLLT could help PNL patients and improve their quality of life.
Subjects and methods
Data sources and literature search strategy
Two independent authors performed a systematic literature search in PubMed, Scopus, Physiotherapy Evidence Database (PEDro), Cochrane, Google Scholar, and Egyptian Knowledge Bank (EKB) databases from 2007 to 2024 using the keywords “LASER”, “low-level laser therapy”, “laser therapy”, “phototherapy”, “photo-biomodulation”, “peripheral nerve injury”, “carpal tunnel syndrome”, “brachial plexus lesion”, and “nerve repair”, with the Boolean operators, “OR” and “AND”. The next algorithm contained the Medical Subject Headings (MeSH) and keywords, ((“LASER” OR (“low-level laser therapy”[MeSH term])” OR “light therapy [MeSH term]” OR “laser therapy” [MeSH term] OR “photo therapy [MeSH term]” OR “photo-biomodulation” [MeSH term])) AND ((“post- surgical [“median\ulnar\radial nerve repair”] OR (“post-surgical peripheral nerve repair”) AND “peripheral nerve [“injury” OR “lesion” [MeSH terms]) OR “neuropathy” [MeSH term]) AND “carpal tunnel syndrome” AND “cubital tunnel syndrome” AND “tarsal tunnel syndrome” AND (“brachial plexus” OR “sacral plexus” OR “lumbar plexus” AND ((“tibial\Sciatic\sural\ peroneal nerve”)) (“cut” OR “repair” [MeSH terms])) AND (“randomised clinical trial” OR “experimental study” [MeSH terms]) [10].
After the search, a number of articles were retrieved from each database and downloaded in the RiS or BiB formats. The files were analysed with the Mendeley Desktop tool, developed for the preliminary selection of abstracts and titles articles (https://www.mendeley.com) [11].
Studies were included if they were published in English and excluded if they had a PEDro score of less than five. Also, the reference lists of the included studies were manually searched to account for any missed records.
Eligibility criteria
For the current systematic review, a clinical question was formulated using the Population, intervention, Comparison, and intervention (PiCO) framework (Table 1) [12]. PiCO comprises data collection, primary and secondary outcomes, treatments administered, comparative treatments, and demographic variables. inclusion criteria were (1) randomised controlled trial (RCT) articles, (2) articles published in English, (3) LLLT as an intervention, compared to either a placebo or another intervention, (4) patients of any age who had PNLs assessed for sensory or motor nerve regeneration through EMG or NCS, and pain. The exclusion criteria were (1) articles published in a non-English language, (2) case reports, crosssectional, cohort, case-control, case series, case studies, and reviews, (3) no LLLT intervention, (4) participants were not PNL patients, (5) in vitro or animal studies, and (6) outcomes assessed were not EMG or NCS and pain.
Table 1
Population, intervention, comparison, and intervention format and search keywords
Screening and filtration
Two authors screened the titles and abstracts of articles against pre-specified eligibility criteria, followed by full-text filtration of the eligible articles to determine the included articles. Any conflicts were resolved after discussion with the senior author.
The main variables of interest were pain intensity and sensory nerve regeneration in PNL patients treated with laser therapy, while motor nerve regeneration changes were a secondary outcome.
Quality assessment
The PEDro scale, a reliable instrument for evaluating RCTs [13], assessed study bias and quality [14]. Each evaluator performed independent assessments, with any disagreement discussed until a consensus was reached. RCTs with a PEDro scale score < 5 were classified as low quality, while articles with scores > 6 were considered high quality. Total PEDro scores are presented in (Table 2).
Table 2
Risk of bias assessment of the included studies
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rochkind et al., 2007 [15] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 9/10 |
| Shooshtari et al., 2008 [16] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5/10 |
| Yagci et al., 2009 [17] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 9/10 |
| Fusakul et al., 2014 [18] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10/10 |
| Zoheiry et al., 2019 [19] | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 7/10 |
| Elgendy et al, 2020 [20] | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 9/10 |
| Atiaa et al., 2021 [21] | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 8/10 |
| Nalbant et al., 2022 [22] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10/10 |
[i] The PEDro scale scores: (1) eligibility requirements, (2) random assignment, (3) covert allocation, (4) baseline similarity, (5) participant blinding, (6) therapist blinding, (7) assessor blinding, (8) intention-to-treat analysis, (9) assessments of at least one major outcome from at least 85% of participants initially assigned to groups, (10) comparison of groups, and (11) point measurements and variability measures A score of 1 indicates “yes”, 0 indicates “no”, and the highest possible score is 10 (criterion 1 is not included in scores)
Statistical analysis
Review Manager (RevMan) version 5.4.1 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark, 2021) was used to examine data from the included studies and perform the meta-analysis. Measures of continuous effects were presented as mean difference (MD) with 95% Ci. A random-effects model was employed due to significant heterogeneity.
Results
Study selection
The initial search of six databases identified 1539 articles, of which 37 full texts were assessed, with eight articles included in the review and meta-analysis.
Most studies published in the current decade originated from five countries, with eight RCTs including a total sample of 397 participants (199 in experimental groups and 198 in control groups). After reading the titles and abstracts, articles that potentially fit the inclusion criteria were selected for full-text review. When there was disagreement between the reviews, a senior reviewer was brought in to help reach a decision. Figure 1 shows the Preferred Reporting items for Systematic reviews and Meta-Analyses (PRiSMA) flowchart used [23].
Data extraction
Study characteristics
The information extracted from the eight eligible articles included reference name, population (number and age), experimental group health condition and intervention, control group intervention, intervention outcomes (frequency or du ration), and results. Table 3 provides a comprehensive summary of the information extracted.
Table 3
Summary of the included studies
| Author | n Age (years) | Health Condition | intervention in EG | intervention in CG | Outcomes | Frequency\duration | Results |
|---|---|---|---|---|---|---|---|
| Rochkind et al. 2007 [15] | 18 10 laser 8 placebo 20-74 | incomplete PNi at different levels for at least 6 months | laser + splint | splint | CMAP Motor Function Sensory Scale | laser 180 min/day to peripheral nerve and 2 hrs/day to corresponding spinal segments 21 days 780 nm | Laser use can substantially enhance nerve function, leading to a full functional recovery |
| Shooshtari et al. 2008 [16] | 80 40 laser 40 placebo 30-70 | CTS | laser | placebo | VAS Ncv | laser at dorsum of hand and palm 5 session/week 15 session 785 nm | Laser therapy for the treatment of CTS paresthesia and numbness was beneficial, with patients reporting increased grip strength and electrophysiological improvements as a result of treatment |
| Yagci et al. 2009 [17] | 45 24 control 21 laser 40-64 | CTS | laser | placebo | CMAP Motor Function Sensory Scale | laser + splint where median nerve is superficial 90 s x 3 points 10 sessions 830 nm | Laser can be used to decrease pain intensity and improve NCV |
| Fusakul 2014 [18] | 112 56 laser 56 placebo Above 18 | CTS | laser + splint | splint | BCT Questionnaire SSS Fss Hand grip Vas Ncv Emg (CMAP) | splint + laser whole wrist crease 5 cm below and above 3 sessions/week for 5 weeks 15 sessions 810 nm | While both laser and splints were effective in alleviating the symptoms of mild to moderate CTS, laser treatment showed electrophysiological improvements in median motor nerve fibre conduction that splints did not |
| Zoheiry et al. 2019 [19] | 30 15 laser 15 placebo 20-40 | post burn ulnar nerve entrapment | medical Treatment + laser | medical Treatment Only | VAS Ncv median and ulnar | laser 15 min medial epicondyle + common flexor tendon and splint where median nerve is superficial 90 s x 3 points 10 sessions 1064 nm | Post-burn individuals with cubital tunnel syndrome benefit from increased ulnar nerve conduction velocity and decreased pain intensity after laser treatment |
| Elgendy et al. 2020 [20] | 40 20 laser 20 placebo 61-43 | CTS | laser + splint | splint | SSS Fss Hand grip Ncv Mcv | laser 3 times\week for 4 weeks 12 sessions wrist crease and ulnar 10 session 905 nm | Laser and splinting provided improvements in clinical parameters |
| Atiaa et al. 2021 [21] | 30 15 laser 15 control 40-55 | DPN | laser + medication | medical Treatment Only | NCV peroneal VAS | laser + medication dorsum of feet, head of fibula, lateral calf 905 nm | Patients experiencing painful DPN reported less pain intensity and better NCV after laser treatment |
| Nalbant et al. 2022 [22] | 42 22 laser 20 placebo 32-65 | CTS | laser | placebo | Phanel and tinel test BCT Questionnaire SSS Fss Ncv median EMG Us | laser over the wrist for 2 min 15 session + splint 670 nm | Enhancements in clinical and electrophysiological measures, as well as enhancements in sensory nerve conduction investigations, were observed in the laser group |
[i] BCT Questionnaire - Boston Carpal Tunnel Syndrome Questionnaire, CG - control group, CMAP - compound motor action potential, CTS - carpal tunnel syndrome, DPN - diabetic peripheral neuropathy, EG - experimental group, EMG - electromyography, FSS - functional status score, PNi - peripheral nerve injury, SSS - symptom severity scale, NCV - nerve conduction velocity, MCV - motor conduction velocity, SSS - symptom severity scale, US - ultrasound, VAS - visual analogue scale
Participants
All participants were adults with carpal tunnel syndrome [20-22, 16, 17], ulnar nerve entrapment [19], traumatic nerve injury [15], or diabetic neuropathy [21].
Interventions
In all studies, the experimental group received laser therapy treatment, with the intervention time ranging from 5 to 15 min at a frequency of three times per week, except for one study [15] in which the patients received 180 min/day across the whole peripheral nerve and two hours on corresponding spinal regions for 21 days. Meanwhile, the control groups received a placebo treatment, splint, or pharmaceutical intervention.
Outcome measures
The studies included in this review measured pain intensity using the visual analogue scale (VAS), nerve conduction velocity (NCV), and compound motor action potential (CMAP). The means of study and control groups and the differences reported are summarised in Table 4.
Table 4
A summary of study and control group results
| Study | Rochkind et al. 2007 [15] | Shooshtari et al. 2008 [16] | Yagci et al. 2009 [17] | Fusakul 2014 [18] | Zoheiry et al. 2019 [19] | Elgendy et al. 2020 [20] | Atiaa et al. 2021 [21] | Nalbant et al. 2022 [22] |
|---|---|---|---|---|---|---|---|---|
| Outcomes | increased nerve function leading to substantial Functional Improvement | SNCV Increased | significant improvements in clinical and Ncs outcomes | grip strength distal motor latency Was Significantly Improved | enhanced ulnar NCV and pain alleviation | median nerve conduction studies improved | reduction of VAS and Substantial Ncv increase | enhanced ulnar NCV and pain alleviation |
| Control Group Means | CMAP pre = 1.5 post = 1.1 | VAS Pre = 8.01 post = 7.62 SNCV pre = 34.07 post = 34.89 | VAS Pre = 8.3 post = 8.1 SNCV pre = 36.56 post=38.86 CMAP pre = 11.2 post = 11.94 | VAS Pre = 4.83 post = 2.48 CMAP pre = 9.9 post = 9.94 | SNCV pre = 43.88 post = 44.62 | VAS Pre = 8.3 post = 8.1 SNCV pre = 29.05 post = 29.1 | VAS Pre = 7.6 post = 7.6 SNCV pre = 45.0 2 Post = 45.02 | SNCV pre = 32.7 post = 32.5 CMAP pre = 7.6 post = 7.7 |
| Study Group Means | CMAP pre = 1.3 post = 1.7 | VAS Pre = 7.8 post = 4.98 SNCV pre = 32.07 post = 34.89 | VAS Pre = 8.04 post = 1.4 SNCV pre = 35.34 post =38.54 CMAP pre = 10.14 post = 10.3 | VAS Pre = 6.26 post = 3.45 CMAP pre = 9.88 post = 9.95 | SNCV pre = 43.91 post = 55.77 | VAS Pre = 8.04 post = 1.4 SNCV pre = 38.1 post = 44.5 | VAS pre = 8 post = 2.8 SNCV pre = 98.8 post = 115.1 | SNCV pre = 31.3 post = 33.3 CMAP pre = 8 post = 8.7 |
| Difference Between Means | CMAP Control = -4 study = 0.4 | VAS Control = -0.39 study = -2.82 SNCV Control= -0.06 study = 2.11 | VAS Control = -0.2 study = -6.64 SNCV Control = 2.3 study = 3.2 CMAP Control = 0.74 study = 0.16 | VAS Control = -2.81 study = -0.2 CMAP Control = 0.04 study = 0.07 | SNCV Control = 0.74 study = 11.8 | VAS Control= -0.2 Study = -6.64 SNCV Control = 0.05 study = -6.4 | VAS Control = 0 study = -5.2 SNCV Control = 0 study = 16.3 | SNCV Control = -0.2 study = 2 CMAP Control = 0.1 study = 0.7 |
Three RCTs with ratings above six on the PEDro scale are the reason for the results of the studies being considered strong (kappa coefficients of 0.90 for consensus generated by two evaluators and inter-rater agreement for PEDro = 81%).
Meta-analysis
The initial search of six databases, including PubMed (n = 291), Scopus (n = 216), Cochrane (n = 198), Google Scholar (n = 355), PEDro (n = 312), and EKB (n = 167), identified 1539 articles. The Mendeley desktop program removed 117 duplicate articles, with only eight remaining after a review of the titles, abstracts, and full texts.
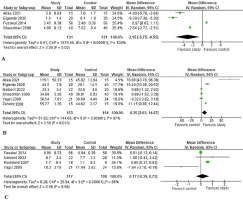
Revman version 5.4.1 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark, 2021) examined the data from the included studies. Measures of continuous effects were presented as MD with 95% Ci. A fixed effects model was not considered appropriate due to the presence of significant heterogeneity. According to Cochrane standards for meta-analysis, the random effects model was employed because the heterogeneity was statistically significant, with an /2 statistic above 50% (as shown in Figure 2). This suggests that the true effect size varied across studies rather than being identical.
Figure 2
Meta-analysis: (A) comparisons of visual analogue scale (VAS) between study and control groups, (B) comparisons of sensory nerve velocity (SNCV) between study and control groups, (C) comparisons of compound motor action potential (CMAP) between study and control groups. Each comparison is presented alongside the name of the first author and publication year
Standard heterogeneity analysis using the /2 statistic indicated substantial variability in effect estimates, which is beyond what would be expected by chance alone. Sensitivity analysis was not applicable in this context, as there was no single study that significantly influenced the pooled results, and the included studies were too different to allow for such an analysis.
Overall, this meta-analysis adhered to the Cochrane standards, ensuring that the methodology appropriately reflects the variability and complexity of the data [24]. Statistical analysis testing with two sides and a 0.05 a-error threshold was used.
Effect of laser on pain
Four studies assessed pain intensity using the VAS in laser and control groups before and after treatment [21,20, 18, 16]. The meta-analysis showed significant improvements in the laser group compared to the control group (95% Ci; /2 = 100%; chi2 = 1578.40; p = 0.02). The studies are described in Figure 2A.
Effects of laser therapy on nerve conduction velocity assessment of nerve regeneration
Six studies used NCV to compare nerve regeneration in a laser and control group [21,20, 22, 16, 17, 19]. Pooled statistical analysis revealed significant improvement in the laser group compared to the control group (95% Ci; I2 = 97%; chi2 = 144.66; p = 0.01). The studies are described in Figure 2B.
Effects of laser therapy compound motor action potential assessment of nerve regeneration
Four studies used CMAP to compare nerve regeneration in laser and control groups before and after treatment [18, 22, 16, 17]. The studies (Figure 2C) revealed no significant differences between the laser and control groups (95% Ci; I2 = 88%; chi2 = 25.94; p = 0.56).
Discussion
The purpose of this review was to systematically assess the scientific evidence for using LLLT as a physical therapy for treating PNL patients. The results demonstrated that LLLT improved pain intensity and nerve regeneration, especially sensory regeneration, but did not affect more motor nerves.
The light used for LLLT falls into an “optical window” at red and near-infrared (NiR) wavelengths (600-1070 nm), as effective tissue penetration is maximised in this range [25].
One RCT was low quality, based on the PEDro scale, while the other seven were high quality, scoring > 7 out of 10 [13, 14].
Pain thresholds increased after three hours of laser irradiation, which may be due to a reduction in nerve impulses caused by a decreased concentration of glutamate channels.
Also, evidence suggests that laser therapy reduces pain by elevating serotonin and beta-endorphin production, as well as acetylcholine esterase activity in synapses [26].
By stimulating cellular respiration through endogenous porphyrins or cytochromes, laser phototherapy stimulates migration and fibre sprouting of neuronal cell aggregates, enhancing the development of large-sized neurons and branched interconnected networks of neuronal fibres. Low-level laser irradiation is also an effective tool for preserving denervat- ed muscle until nerve sprouting into the muscle occurs [27].
Consistent with our finding that better outcomes are associated with quicker recoveries, the results showed that LLLT is an effective, safe, and appropriate alternative treatment for facial nerve palsy, especially in cases where traditional drugs like corticosteroids present too many risks, such as diabetes (e.g., hyperglycaemia) [28].
Our findings show that those treated with LLLT had far greater signs of reinnervation, substantially greater muscular power, and no negative side effects [29].
In contrast to our findings, previous work [30] found that laser therapy substantially enhanced the amplitude of neuronal potentials in individuals experiencing pain by acting on sensory axons indirectly. The increase in the neural potential amplitude after laser therapy may be associated with pain relief in patients with painful diabetic peripheral neuropathy (DPN). However, it had no direct influence on sensory conduction velocity (SCV) or motor conduction velocity (MCV) in DPN patients.
Our results contradict earlier research showing no difference between laser and control groups in the two-point discrimination test [31]. Neither group had improvements in their thumbs, though there was an improvement in the index finger of those receiving LLLT. However, muscle tests, including opposition and thumb abduction, showed substantial improvement in the laser group, who also had marked motor improvements demonstrated by EMG and NCV. Consequently, some nerve growth parameters appeared to be influenced by laser therapy, mostly on motor rather than sensory fibres.
Despite our results demonstrating LLLT efficacy, the study had significant population heterogeneity. As such, the absence of subgroup homogeneity is a limitation of this metaanalysis. There was also significant clinical heterogeneity, with five studies involving adults with carpal tunnel syndrome [16-18, 20, 23], one focusing on ulnar nerve entrapment [21], another on traumatic nerve injury [19], and one on diabetic neuropathy [22]. The high overall heterogeneity observed in the meta-analysis may be influenced by these clinical differences. The statistical heterogeneity (I2 = 100, 98 and 88%) may be caused by variations in the study populations, tests used, and reference tests, which can all result in different estimates of diagnostic accuracy and introduce bias into the metaanalysis. Most RCTs involved single lesion nerve repair, carpal tunnel, or tarsal tunnel, with few measuring MCV as an outcome, which reflects the progress of nerve regeneration, so obstructs holding it in another meta-analysis.
Conclusions
This systematic review analysed eight RCTs using strict inclusion eligibility criteria. The current evidence supports using LLLT to improve pain intensity and sensory nerve regeneration but not motor regeneration. Nonetheless, the evidence for LLLT effectiveness in motor regeneration can be considered moderate. While this analysis does suggest that laser treatment is beneficial for PNL patients, further RCTs with a larger sample size are needed to support these findings.
Limitations
The review focused on comparing LLLT with alternatives (placebo, splint, or medication) in PNL patients. However, the meta-analysis was not attainable for more studies as there were not enough RCTs on this subject. Also, the small sample size in the selected studies limited the ability to draw general conclusions.
The outcomes were limited to pain, SNVC, and CMAP since too few studies measured NCV to allow for a metaanalysis. This review established that LLLT had no significant effect on CMAP in PNL patients compared to placebo. Furthermore, the review was limited by the lack of a sensitivity analysis to address meta-analysis heterogeneity.


